SCOTCAP SERVICE MODEL EVALUATION
SCOTCAP is a potential new shared service model for a video
capsule endoscopy in Scotland which compliments existing endoscopy services
EXECUTIVE SUMMARY
‘SCOTCAP Service Model Evaluation’ is a collaboration between Scotland’s Digital Health & Care Institute (DHI) and NHS Highland, NHS Grampian and NHS Western Isles running from May 2019 till March 2020, during the SCOTCAP Innovation Phase. The project was sponsored by the Scottish Government.
The collaboration was proposed as a new and innovative way to design, evolve and establish a new healthcare provision in endoscopy services. If successful, the new video capsule endoscopy service, hereon known as SCOTCAP, would bring a new product and service to the ‘family of colonoscopy services’ underpinning existing activities and in time, offering a new choice of service for patients who may not require a full colonoscopy.
The DHI Design Team, led by Design Researchers from the Glasgow School of Art (GSA) Innovation School, are experts in design research for complex environments, and were commissioned to work with the project partners to explore how each Health Board (HB) adopted, integrated, and ran, the managed service model during the SCOTCAP Innovation Phase, and to produce recommendations to support the full integration of SCOTCAP within existing NHS services for gastric patients in future. To meet these aims we led co-production design-based processes with each of the HB teams, the Medtronic/ Corporate Health International (CHI) Partnership and a broad spectrum of stakeholders.
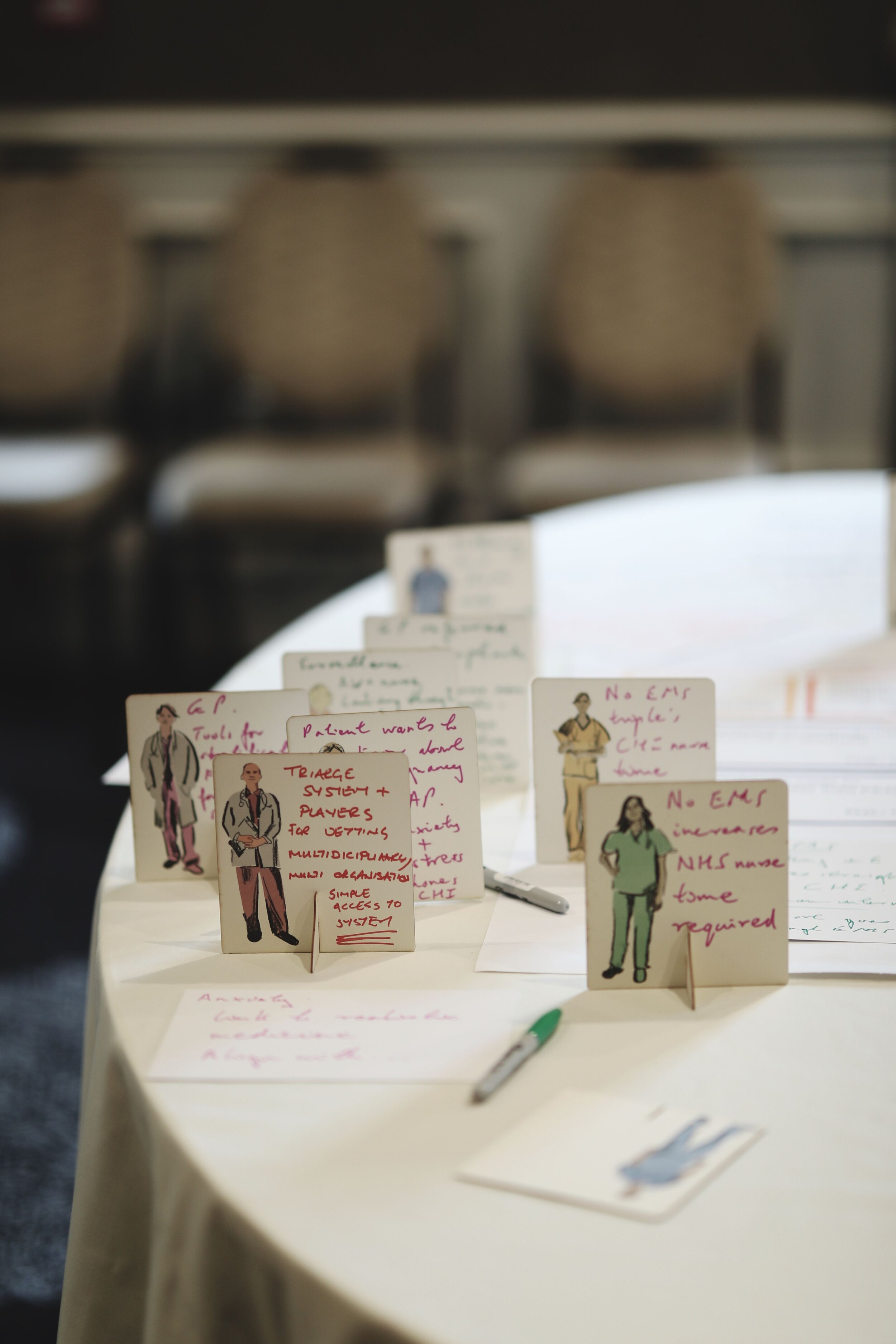
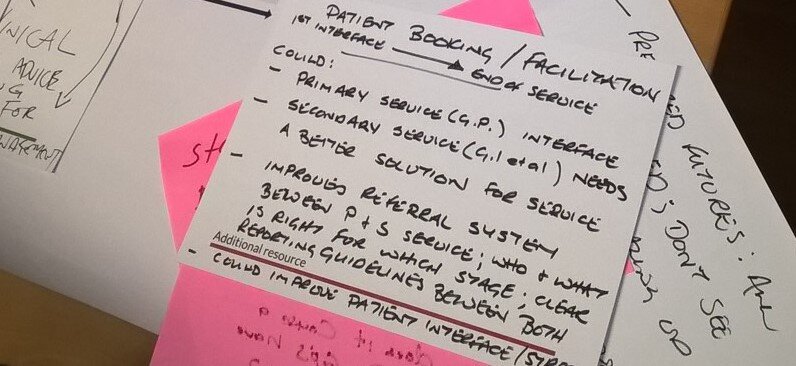
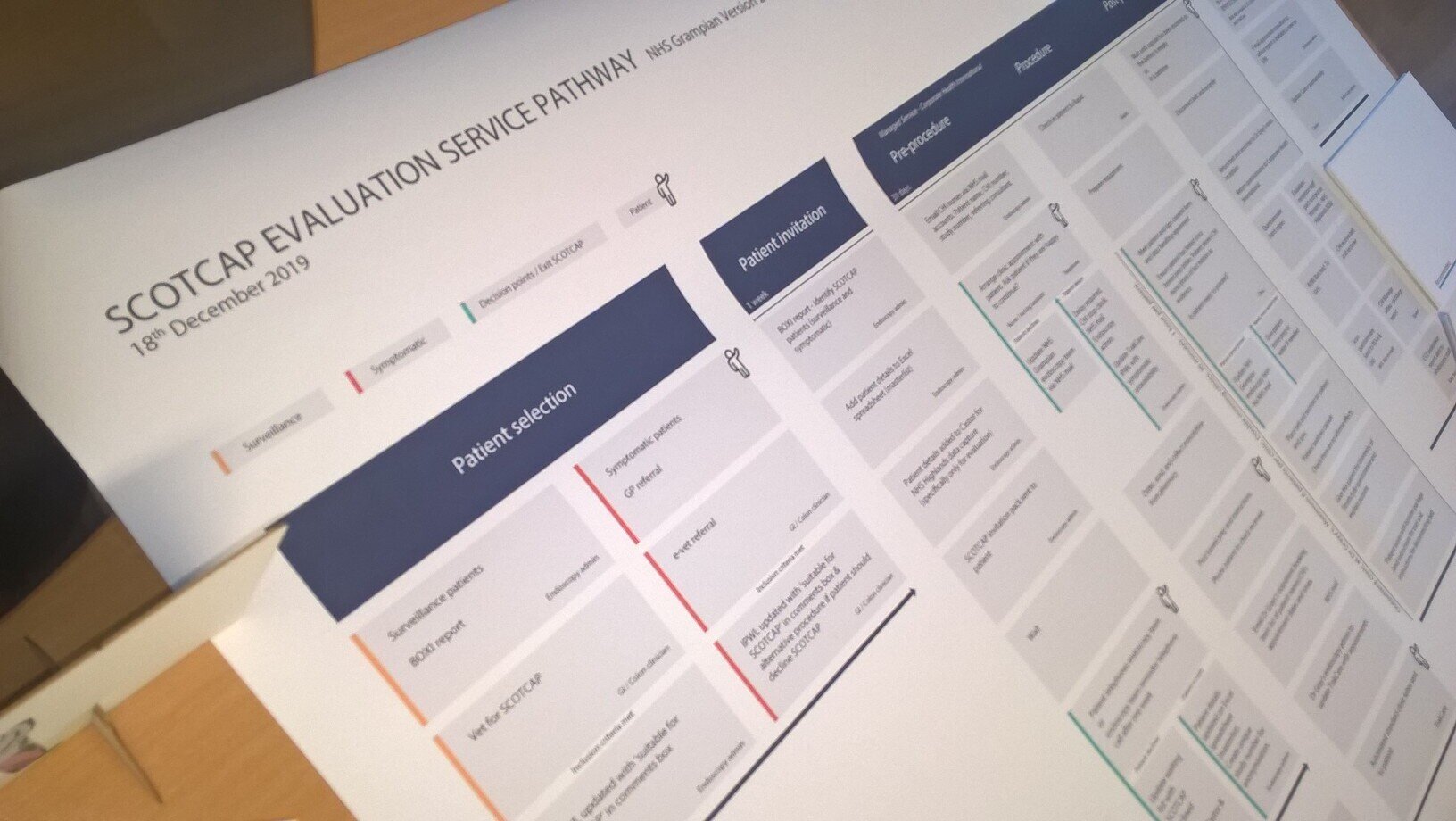
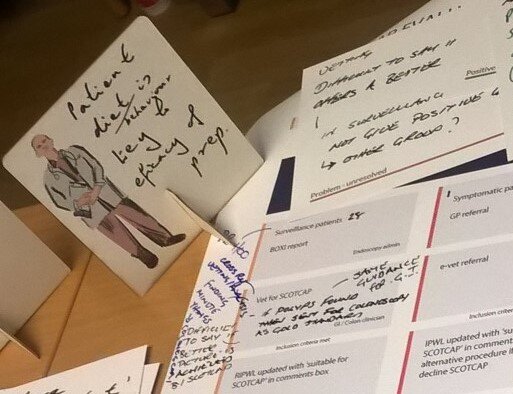
Initial interviews with key participants were undertaken to gain a rich understanding of the current state of the service model and inform the next stage of the project, the co-design workshops. Key professionals from the participating HBs were invited to a workshop to explore the respective SCOTCAP service models associated with their role. Design-led methods and tools were used with participants to map the service model and the key sub service pathways (patient invitation etc). Using record cards, post-its and service model maps, participants discussed and recorded the challenges incurred during the initial service interfaces, the opportunities these presented, and key recommendations to improve and scale-up the service model if this were to be used by other HBs. Outputs from these activities were then analysed using various techniques, such as group wall analysis and audio transcription analysis, to synthesise and identify key issues, ideas, and concepts which later led to key themes for the project.
Outputs from this research project (Service Model Blueprint and Report) offer key recommendations and visualisations of how SCOTCAP as a service could progress in future.
“we are doing an expensive test (colonoscopy) for a lot of normal people
”
KEY RECOMMENDATIONS
CULTURAL CHANGE AT THE ORGANISATION LEVEL
In order for SCOTCAP to be a success, and adopted at scale, a culture of change is required to achieve the level of organisational and service change that enables the integration of the SCOTCAP service within existing NHS services. A revision of service delivery mechanisms across the gastroenterology health service ecosystem (e.g. best use of services such as colonoscopy, SCOTCAP, dietitians etc.) is advised, building on service improvement work already underway within the Scottish Government. This would entail working collaboratively with various Organisations on a number of levels (National/Health Board/Private) to enable sustainable, service improvements in many service areas.
Recommendations include:
Strong leadership, governance and clarity across the relevant participatory Organisations regarding contribution of CCE to service delivery model;
If achieved a clear message to staff at all levels of organisational and service delivery which should enable the cultural shift required to make the step changes in this new diagnostic service model for GI;
Any new service model should consider opportunities for new workforce models, changes to job descriptions, training and a revision of staff workloads.
ELECTRONIC ENDOSCOPY MANAGEMENT SYSTEM (EMS)
The introduction of EMS should be a priority for the next stage of the project to ensure workflow and referral management are
optimised and effective. The system should have the design and capability suitable to meet the varying needs of all professionals to access the service. It should also be an intuitive system with a seamlessly interface with other NHS ICT systems. Clear national policy and guidance should be identified which supports specifically the adoption and delivery of the SCOTCAP service. It is recommended that an integrated referral management solution for Capsule Endoscopy such as EMS be made available Nationally, which will avoid information duplication and optimise efficacies if the CCE service model is adopted at scale.
Additional key system recommendations include:
Be a national system with an integrated CCE portal (tab);
Interface with TrakCare and other NHS systems;
Support National guidelines developed for SCOTCAP;
Include vetting criteria and information as part of the Endoscopy service offering building in referral to CCE as an option;
Be cloud-based;
Be GDPR compliant;
Allow real-time access;
Allow sharing of data between Primary and Secondary Care.
COMMUNICATION CHANNELS
There is an opportunity to streamline and attune communication channels and systems by reviewing and synergising current communication methods (ICT & human) at various communication stages along the pathway (e.g. Patient – NHS; Patient- Managed Service Provider; NHS – Managed Service Provider). During the Innovation Phase some misunderstanding and frustration was caused by misaligned communication mechanisms and lack of integration (ICTS & processes), different professional terminologies and various ‘best practice’ approaches.
CLUSTER SERVICE MODEL
Participants agreed greater interactivity between Primary and Secondary Care is required for scaling up of SCOTCAP and associated services to run successfully. A cluster approach was considered the optimum service model for SCOTCAP based on a GP-led service
located in community hubs or community buildings. It was agreed that at this time further evaluation and exploration was required before an at home service delivery model could be considered.
VETTING
A new digitally enabled vetting system which reviews, sorts and identifies the most appropriate service pathway for all patients reflecting their specific needs and circumstances should be undertaken for the next stage of the SCOTCAP project. This new vetting approach should be used for:
All GI referrals, including endoscopy referrals (symptomatic/surveillance/screening); and,
Should work from clear national guidelines to ensure transparency in deciding the ‘best route to care’ for patients that practitioners should follow i.e. considering factors such as FIT & Indicators (rurality or accessibility profile, dependencies, work commitments, other health criteria and history, patient views, and ability to take bowel preparation).
This would work to address the early idiosyncrasies observed in the SCOTCAP Service Model Innovation Phase across the Health Board Areas.
NATIONAL PHARMACY DISTRIBUTION MODEL
Participants indicated during preparation stages that potential variations between participating Health Board’s approaches to pharmacy dispensing and distribution of products would be a significant challenge for the project.
The management of pharmacy arrangements for each of the three participating Health Boards was similar for the Innovation Phase of the project and coordinated via NHS Highland Pharmacy. However, it was clear from engagement with NHS Grampian Pharmacy colleagues that this arrangement with NHS Highland would not be a sustainable approach or be suitable for national scale up.
It is recommended that a new centralised dispensing and distribution model be developed, potentially with a National Pharmacy Organisation dispensing on behalf of NHS Boards, ensuring compliance with national agreed standards and dispensing regulations. This could facilitate the dispensing and distribution in the short to medium term of the following:
Bowel preparation products.
Personalised guidance, instructions to support bowel cleaning, and key contacts.
TECHNOLOGY INNOVATION
Participants endorsed the use of an Innovative Procurement Partnership to drive innovation, a route to market and value for money (VFM) for the SCOTCAP project. Currently lack of market competition was identified as the main cause for little development of the technologies currently used in the managed service. It was hoped that as the SCOTCAP service gains pace this will:
Act as a driver for change in technology development (improvements in the size of the receiver, video camera capsule and battery life (currently a maximum of 12hrs).
Use Innovative Procurement Partnership approaches to drive greater economies of scale in technology purchases for the scaled model.
These outcomes would support an improved patient experience (smaller capsule) and VFM in the service delivery.
BOWEL PREPARATION & PATIENT SUPPORT
Effective bowel preparation and cleansing is essential for a successful CCE but relies on patient adherence and ability to undertake the process independently.
Patients should be screened for their ability to undertake this process effectively and only those considered suitable should be invited to the SCOTCAP service.
Patient support methodologies (written and remote support) developed for the Innovation Phase should inform national guidelines to support wider adoption at scale.
Co-produced patient information should continue to be used to ensure easily accessible information is available (digital and/or hard copy) to optimise the patient experience and support.
BELT MANAGEMENT
Different models to support belt and recorder delivery and return from the patient have been considered as part of the Innovation Phase Service Model Evaluation. However, to enable at scale adoption and mitigate the risk of lost equipment/ data and delays in returning the equipment, alternative service delivery models should be explored to ensure suitability for a National model involving greater numbers of transactions. Non-NHS courier services or returns via local community pharmacies were suggested as options by participants. The option to use a digital resource such as a cloud-based system, to upload data directly from cluster hubs to the SCOTCAP server was suggested by participants as a longer-term action.
RESEARCH
The SCOTCAP Service Model Evaluation research evidences the process of designing and optimising the SCOTCAP service model, and how this relates to the wider continual evolution of an at scale service model beyond the Innovation Phase. Good insights have been gathered from the NHS Highland Board Area but due to time pressure and later starting dates of the SCOTCAP Innovation Phase in the other participating Health Board Areas more limited and provisional evidence has been gathered from them to inform this report. It is therefore recommended that:
It is anticipated the SCOTCAP service model and its interface with the wider ‘colonoscopy family of services’ will go through further alterations and refinement towards development of a National Service Model;
Further research and evaluation should be undertaken to evaluate the new changes to the SCOTCAP service model as it extends to other Health Boards;
This should continue to include an evaluation of the service model, patient experience and health economics.
OUR APPROACH
PROJECT AIMS & Objectives
The aim of the project was to support the development of the SCOTCAP service model through a design led co-production approach.
The key goals were to identify and map out current service models for each Health Board area, explore the key challenges, opportunities, and recommendations with the respective professionals in delivering this new service, and develop key recommendations for a service model blueprint and report.
As this project has adopted a proactive, evolutionary approach, with constant adaptive updates by the team as events unfold, some of the recommendations may be in progress. This report and associated service model blueprint act as a marker of developments up to March 2020.
We sought to understand and gather evidence which elicited insights to establish:
What can be copied over from the SCOTCAP Service Model Innovation Phase to the future SCOTCAP service?
How does the SCOTCAP Service Model Innovation Phase delivery vary between the three participating boards?
How would the future SCOTCAP service delivery vary between NHS Scotland’s boards?
The additional resource requirements for implementing the SCOTCAP service which will inform indicative costs.
The delivery of some of the outcomes (predominantly cross and sub organisation & technology) may have to take a measured staged approach due to current processes and management arrangements, the dexterity to change, and the ability to deliver the more complex recommendations. It is suggested further design support should be considered at the next stage of the service model development to enable the higher level innovative discussions to continue and bring greater insights for a national model.
WHAT WE DID
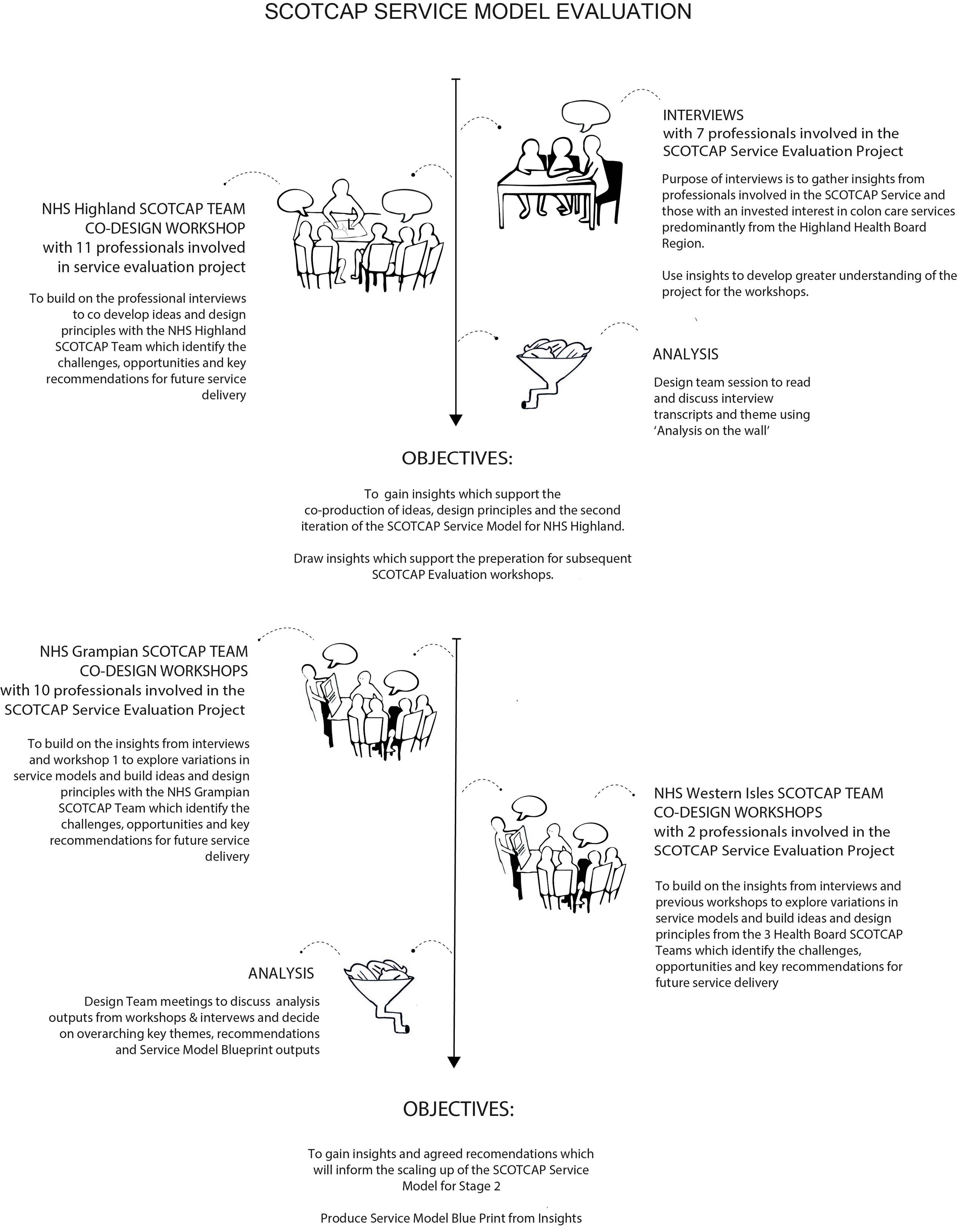
The Glasgow School of Art (DHI Design Team) were tasked with evaluating the SCOTCAP Service Model during the Innovation Phase and make evidence-based recommendations for a future service model in the form of a Service Blueprint. Interviews with professionals involved in this project from the NHS Highland Health Board were undertaken to inform the subsequent workshops with the three Health Boards involved in the project (NHS Highland, NHS Grampian, NHS Western Isles). The NHS Highland delivery team was the earliest established in the Innovation Phase of the three HBs and therefore insights from this group would offer the most significant insights at the early stage of the project. The service delivery would be a managed service model and therefore key professionals from both public and private organisations were invited for interview.
Six individuals were invited to interview (Senior NHS Consultant; NHS Service Manager; Managed Service Delivery Manager; Managed Service Director, Private Sector Health Service Manager, Third Sector Bowel Care Manager). One-to-one semi-structured interviews were conducted in person and/or by telephone.
Topics of discussion included:
Organisational Change (National – Local)
Technology capabilities and limitations
Limitations of current colonoscopy service
Challenges in delivering the SCOTCAP service at key service pathway points
Opportunities for the future
Delivering the service ‘at Scale’
Co-design Workshops
Co-design workshop 1: Of the three participating Health Boards, NHS Highland Health Board and the Medtronic/ CHI partnership had actively been running a SCOTCAP Service Model Innovation Phase the longest and had the largest number of patients on the project. A co-design workshop was run with 11 professionals involved in the SCOTCAP project, including Endoscopy practitioners, NHS administration nurses, the CHI managed service team, Medtronic representatives and professionals from primary services. The co-design workshops used various design tools (current service pathway map, prompt cards, response cards (problems resolved, problems unresolved, positive outcomes, key recommendations). The aim of the workshop was to identify participant’s views on the challenges they have experienced with the service during the Innovation Phase, what improvements could be made, key recommendations for a future service, and what would be needed to deliver the service at a national scale. ‘Talking Heads’ interviews were also video recorded with key professionals to add rich insights to the research findings.
Co-design workshop 1 (NHS Highland Board):
A whole day co-design workshop was held at the Kingsmill Hotel, Inverness, where participants were taken through the current
state map of the NHS Highland SCOTCAP service model and asked to focus on key stages (patient selection, patient invitation, pre-procedure, post-procedure and report), to discuss key issues and share ideas.
SESSION 1
Service Model Delivery
Good things that should be recommended to other HBs and should be copied to the future SCOTCAP service;
Problems that have been resolved (to capture learning);
Problems that are unresolved (still being done in a way that can’t or won’t be done in the future SCOTCAP service); and,
SESSION 2
Cost and Benefits
Additional resources. Identify staff and systems that would be extra cost or resource above and beyond the current endoscopy service.
Positive outcomes. Identify benefits at the current stage of the SCOTCAP Innovation Phase (may have to be anticipated).
SESSION 3
KEY RECOMMENDATIONS
Key recommendations to be taken forward for a National Service Model and modes of delivery (e.g. Primary & Secondary service delivery model, patient support, etc.)
Co-design workshop 2 (NHS Grampian Health Board):
A whole day co-design workshop was held at the Dr Grays Hospital, Elgin, and the same process adopted in co-design workshop 1
was followed with participants for NHS Grampian. The only deviation from this approach was a two half-day approach to work around the work commitments of the participants. Insights from the early interviews, NHS Highland co-design workshop and the inclusion of an NSS representative added a progressive tone to the interactions, particularly identifying commonalities and recommendations.
Co design workshop 3 (NHS Western Isles Health Board)
A co-design workshop was held at NHS Western Isles hospital, Stornoway, and low numbers of available attendees was a
result of multiple commitments to island service delivery and the limited timeframe the SCOTCAP service had been ‘live’. The
same approach was adopted as with workshops 1 and 2 drawing from earlier insights where applicable. Workshop insights were supported by a 1:1 interview with the lead colonoscopy professional and in addition to personal insights discussion of the key points identified from previous insights were explored. Though in the early stage of the project insights echoed those from other interactions, albeit with distinct local nuances.
Audio from the interviews and co-design workshop 1 was recorded and transcribed in order to gain rich qualitative data on the service model. Workshops 2 and 3 were not recorded due to institutional ethics boundaries, however, transcribing was undertaken during the workshops, recorded on the service map and feedback cards, and analysis was completed timeously to capture insights as clearly as possible.
Findings
12 Key Challenges and 11 Opportunities were identified as an outcome of the semi structured exploratory interviews and workshops. Some of the challenges identified by participants during the co-design process were specific to the nature of the Innovation Phase, or associated data collection for the Evaluation of the service, but provide useful provocation to discuss opportunities for further learning and development of a fully integrated service. Throughout the Innovation Phase, adaptions were made to resolve challenges as they occurred where possible. Others have been highlighted as opportunities for future exploration.
OVERALL FINDINGS
Initially 15 themes were determined from analysis of the early stage interviews. A further desktop review of these themes established six higher level and 15 sub themes. These themes (Higher level and Sub level) were then regrouped to ‘tell the story’ of the SCOTCAP Service Model Evaluation. These outcomes include recommendations drawn from the narrative which inform how future scaling of the SCOTCAP service could be achieved.
THEME 1: REASONS FOR SCOTCAP IN THE FUTURE
MOTIVATION: The workshop participants agreed that resource constraints, political drive, socio-economic pressures, technology innovation and availability and cultural influences (social & organisation) were collectively driving the need for an improvement in service delivery for GI services. In this respect the current alignment of ‘political will’, ‘resource pressure, ‘technology readiness’, ‘true innovation’ and ‘creating true economic value for Scotland’ were drivers for change.
Waiting times under the current NHS service model for colonoscopy/ endoscopy services were considered to be ‘unmanageable’. Waiting times in one particular NHS Health board were up to 30 weeks, missing both local (4 weeks) and national (6 weeks) targets.
“‘we need to ensure patients are not clinically suffering with our delay in waiting times and we’re able to have a review using the capsule’
”
The SCOTCAP service was viewed in a number of ways, first as additional service which could support meeting the ‘national targets’ for colonoscopy services and, second, by offering greater choice of services that could meet ‘a different type of patients needs’. For the patient this could be a double win, they receive a more timely response from the NHS and have a ‘group’ of choices
that could improve their experience and simultaneously be more personalised service.
Perceptions of the SCOTCAP service was that it could underpin and become part of a ‘family of colonoscopy services’. The most obvious service route for SCOTCAP was seen as offering a level of service to patients who have non-critical health needs, currently many of these patients remain on long waiting lists. If successfully integrated with existing colonoscopy services, this could potentially release NHS service capacity for patients with more critical needs. For example, free up more time for clinical specialists and the support teams (administration, dietitians, etc) to see the high risk/ urgent patients.
LIMITATIONS OF CURRENT SERVICE
Participants felt the cost of the NHS Colonoscopy Services would increase, a ‘business as usual’ approach was not seen as an option, both in the short and long term. An additional service provision which underpinned current and future care needs, such as SCOTCAP, was seen as a good way forward to support an improved service, improve patient experience and make cost reductions. Whilst initial costs associated with a SCOTCAP service were seen as favourable, it was recognised that a comprehensive ‘whole service cost’ for both services was required.
In addition, the introduction of SCOTCAP may counterbalance low uptake of colonoscopy procedures for patients, overcoming issues associated with patient bowel preparation administration, significantly reducing patient travel to and from appointments, avoiding ‘time out’ of daily commitments (work, care), and avoiding potential overnight stays, by offering a less invasive procedure as a choice to patients that meet the vetting criteria.
STRATIFICATION OF COLONOSCOPY SERVICES
A stratified pyramid based approach towards vetting patients for colonoscopy and related services (surveillance/symptomatic/ screening)[1] should be adopted whereby, all patients are ‘sorted’ and identified for the best service which meets their care needs. The Faecal Immunochemical Test (FIT or qFIT) should be part of this along with other indicators such as remoteness/ transport, health and care circumstances, and commitments (work, carer). In this way, CCE can be more targeted and only the most suitable patients would have a full colonoscopy.
[1] Definition of surveillance and symptomatic patients (SCOTCAP Evaluation Protocol):
Symptomatic patients: Undergone a Faecal Immunochemistry Test (FIT) Full Blood Count (FBC) and serum biochemistry test and results available who have been referred by their GP to hospital for further assessment of lower gastrointestinal symptoms e.g. change in bowel habit, rectal bleeding, abdominal pain, weight loss, symptomatic anaemia, presence of an abdominal mass
Surveillance patients: scheduled for a surveillance colonoscopy. The patients may have a personal or family history of colorectal cancer, a history of colonic polyposis or HNPCC.
“‘ I think FIT test is certainly where we want to stay as first line of test for screening’”
Theme 2: COMMUNICATION
LANGUAGE & UNDERSTANDING
Throughout the analysis process it was apparent that there was no common language used to discuss the project. Those involved in
the service delivery across different Health Boards spoke from their own ‘professional language palette’ i.e. their professional experience which could be in contrast to other practitioners. Variability was seen in each ‘section’ of the service model (e.g. patient invitation or procedure pathway) depending upon the actors involved in each task and local services. This was a cause for some misunderstanding and misinformation during the Innovation Phase both with those on the project and external parties (NHS and beyond). For example, describing the SCOTCAP project as an evaluation rather than trial or phrases such as an ‘old’ ‘traditional’ or ‘current’ colonoscopy service.
COMMUNICATION CHANNELS
Multiple communication channels all with differing and nuanced requirements were apparent across the project. These could be grouped in to Patient to NHS; Patient to Managed Service Provider; and NHS to Managed Service Provider communication channels. Interviewees each had pertinent views of ‘best practice’or ‘poor practice’ in this respect.
Participants highlighted communication systems between the patient and service delivery teams (NHS & Medtronic/ CHI) had been framed by existing/ available communication systems and methods that were available at the start of the project. Whilst not ideal, most recognised that these approaches were adopted as part of the pilot as workaround solutions in light of no Endoscopy Management System (EMS) being available. Some limitations and frustrations associated with the various across systems limited communication channels was evident across the project.
PATIENT INFORMATION
It was felt patients should have a clear understanding of the services (SCOTCAP, colonoscopy, endoscopy, etc.) in order for them to make informed choices. The ability of patients to understand and follow instructions, particularly those associated with the bowl preparation, was seen as pivotal to a successful SCOTCAP service. It was evident that a heightened level of instructions, guidance and support was required which worked with the varying abilities of patients to suitably follow instructions. For example, literacy skills which are affected by socio-economic, genetic (dyslexia), age and/ or experience. Communication should be well thought out and considered using multiple methods (technology and human) to ensure the most appropriate and accessible route is adopted.
Patients should be offered realistic options for their patient care pathway based on age related, home situations and healthcare options.
Theme 3: BENEFITS
SERVICE BENEFIT
Participants recognised the SCOTCAP service could reduce the number of patients attending clinics at acute hospitals, which in turn may be more convenient, reduce stress and enable an optional service closer to home. This could alleviate pressure on the larger hospitals by ‘freeing up’ service capacity for those most in need of a full colonoscopy. The CCE technology also has the added value of a more detailed view of the whole gut, including the right-hand side, often an issue for traditional colonoscopy methods, reduce patient waiting times, enabling earlier access for the care pathway.
“‘I would take an alternative if they could stay at (or be closer) to home’
”
“Travel across the Western Isles is an issue, patients would rather not travel ”
PATIENT BENEFIT
A number of benefits for patients would be realised if SCOTCAP was to become part of the ‘Colonoscopy Family of Services’. If the
‘optimal patient group’ can be deciphered for the SCOTCAP service then the following future benefits could be achieved:
A reduction in patients who progress to having an invasive procedure (e.g. no tube inserted in to the body)
The removal of sedation, only a colonoscopy requires this procedure.
A more supportive, local service closer to home.
Reduction of patient stress, anxiety and long waiting times associated with appointments in larger hospitals.
Targeting low uptake patients could increase number of patients seen and in turn improve overall health and life quality and longevity of patients.
Offers a service to those who may otherwise be ‘missed’ ‘delayed’ by lack of capacity of existing services.
‘Closer to home’ service means greater ability for patient to manage ‘day-to-day’ life commitments such as care commitments (e.g. childcare, elderly relatives), work, impact of bowel preparation, etc.
Patients would reduce travel time and waiting time, a higher degree of flexibility.
THEME 4: MANAGING A MANAGED SERVICE
STRATEGIC CONSIDERATIONS
The evaluation process has been seen as valuable in terms of exploring a new innovative Fully Managed service in a different way which allows an evolutionary and adaptable approach, and is supportive of a cautious and pragmatic approach to ‘rolling it (SCOTCAP service) out’ .
“it (the evaluation approach to developing a new service) has offered the possibility to say it’s not working
”
PATIENT SELECTION
Developing a ‘standardised agreed approach’ for patient selection was seen as pivotal to the success of SCOTCAP and ‘the family of colonoscopy services’. This approach would avoid the risk of service duplication and current trend for the overuse of colonoscopy services (currently many patients receive colonoscopies who may not require this service). Patients should be selected for the right reasons for both the patient and service delivery.
The SCOTCAP service should be considered concurrently with other pertinent diagnostic and management services (colonoscopy) at the beginning of their patient journey. Selection could then respond more appropriately to patient needs (low risk, high risk) and if further investigation was required the patient could then be directed for further investigation (colonoscopy or further tests). The evidence from the SCOTCAP project will provide important insights into patient eligibility and suitability and it was felt that further investigation was required to explicitly understand this.
BOWEL PREPARATION
Is seen as ‘absolutely key’ for SCOTCAP however this is a major challenge for the service team to ensure the patient has administered the bowel preparation to the highest standard. Medtronic/ CHI have been developing ‘best practice and support’ in achieving this in co-operation with patients and learnings should inform further approaches. Participants agreed a standardised national agreed approach should be developed for this stage of the SCOTCAP Service to ensure ‘best practice’ is formulated.
THEME 5: THE BIGGER PICTURE
SCALING UP ORGANISATION(S)
Participants spoke of a number of challenges which required consideration if a ‘scaled-up’ version of SCOTCAP is to be achieved. Fundamental will be the need for good Governance and Knowledge Exchange for the next phase of SCOTCAP to ensure that other Health Boards do not ‘recreate the wheel’.
Participants felt that the right processes and systems should be in place that manage external pressure and expectations. e.g. manage local and national aims and objectives with differing often conflicting pressures (Performance Indicators, deadlines, national and inter-departmental objectives and varying deliverables).
A number of ‘risks’ were identified which would impact on an effective and efficient managed service model such as weak points in service delivery across the pathway due to complex interfaces between players and service delivery teams such as manual handovers between NHS professionals, and between NHS professionals and the Medtronic/ CHI team and then back to the NHS teams). The suggestion of a Scottish Passport for private companies who work across Scotland to ensure easier data sharing and importance of using an integrated referrals system such as an EMS was made.
In addition, in order for SCOTCAP to be a success a culture of change is required to achieve the level of organisational service integration required with NHS services. Any new service model should consider new workforce models, changes to job descriptions, training and a revision of staff workloads. During the Innovation Phase staff managed the SCOTCAP service over and above their ‘day jobs’. Alternative suggestions for the SCOTCAP service model were raised by participants especially related to the development of a GP- led, managed service model (or a hybrid of both models).
SCALING UP OF TECHNOLOGY
The technologies used in the SCOTCAP service were limited in terms of their functionality and accessibility and were largely manual based. Several different Information Communication Technology (ICT) systems were used (TrakCare, CHI systems) many of which
required work around solutions (human and technology) to ensure the SCOTCAP service could be achieved. The lack of an integrated EMS system with functionality to support referral management and uploading of reports was seen as a significant barrier. This had been planned as part of the roll out but was not able to be implemented in time. Sharing and retrieving the right document with the most suitable information for each professional was challenging and only achieved through manual means and the good will and effort of those involved.
“‘Unfortunately the system doesn’t give him (endoscopic professional) everything he needs (for vetting)”
In addition, and more specifically, participants recognised that alternative arrangements for sharing the recorded data from the SCOTCAP belts would be required to support a National service. Rather than patients collecting and returning belts to hospitals and GP Practices, SCOTCAP Hubs and cloud-based systems to upload data could form a new business model with data uploaded to a server from the community practices. Good broadband and trained staff would be a prerequisite for this. A streamlined ICT and associated service management plan was suggested to ensure the smooth transition and running of the SCOTCAP service at scale. This could include the management of the patient information and invitations, video data recorded by the SCOTCAP belts and reports.
LIMITATIONS OF DEVICE
It was hoped that as the SCOTCAP service gained pace this (and other drivers for change) would ensure improvements in the size of the receiver, video camera capsule and battery life (currently a maximum of 12hrs). It was also suggested that greater economies of scale could be expected which would lead to reduced costs in the near future. These outcomes would support an improved patient experience (smaller capsule) and Value for Money (VFM) in the service delivery.
THEME 6: THE FUTURE: SCOTCAP AT SCALE
EVIDENCE OF EVALUATION
At this early stage of the evaluation process most interviewees felt that the VFM required a more comprehensive understanding. Views expressed identified the need for all the SCOTCAP service evaluation data to be shared and cross examined to ensure a full understanding was gained (patient experience, level of innovation, optimum service model, business model and management plan). Achieving this would enrich and build a holistic perspective of the SCOTCAP service, and contextualise this within the wider colonoscopy services, building a substantive business case for the next stage. In terms of service delivery, it was acknowledged that SCOTCAP should be considered a ‘disruptive service innovation’ and that the evaluation process not only introduces a new product and service to the NHS but is offering valuable insights which will support improvements across the NHS colonoscopy services through a supportive data gathering exercise.
SERVICE MODEL BLUEPRINT
An interactive version of our Service Model Blueprint can be viewed by clicking on the image below.
NEXT STEPS
LONG TERM
The evidence gathered identified several areas for careful consideration to ensure the SCOTCAP service realises its full potential and the service model can be adopted and delivered at scale within the family of colonoscopy services.
First, as mentioned, scaling up the SCOTCAP service would drive greater economies of scale and bring costs down. Second, interviewees also recognised the inclusion of the managed service was enabling service model innovation both in the NHS and via the Medtronic/ CHI partnership. It was felt without this partnership the project would not have progressed ‘at pace’ nor to it’s current position. This should be corroborated by the Business Evaluation aspect of the current project.
DATA MANAGEMENT
Participants recognised that the future management of data required careful consideration. First, key owners of the data need to be identified in the next phase of the project (will this remain with current research partners, is it funded by UK Grants, NHS or CHI). In order to answer these questions, it is pertinent that partners decide specifically what information is required and who will be tasked with the collation of this information. Part of this future discussion should include the use of Artificial Intelligence (AI). Though this may a be controversial discussion, some participants have offered insights which indicate potential advantages of including this technology, such as the use of AI in video data analysis (this is considered faster and more effective than human analysis). However, if included a clear case must be made and fit for purpose management systems in place. Some interviewees felt greater productivity could be achieved in both SCOTCAP and wider Colonoscopy services and associated time and cost savings if these actions were implemented.
Images from NHS Highland SCOTCAP Workshop attributable to Louise Mather.
AUTHORS
Project Lead Michelle Brogan, Service Development Manager, Digital Health & Care Institute (DHI)
Design Lead Dr Jay Bradley, Research Fellow, The Glasgow School of Art (GSA) - DHI Design Team
Lead Author Dr Megan Palmer-Abbs, Research Fellow, GSA - DHI Design Team
Cate Green, Production Manager, GSA - DHI Design Team
Angela Bruce, Research Associate, GSA - DHI Design Team
Louise Mather, No Middle Name Creative, Photographer and Videographer
Copyright
This publication is copyright. Apart from any use as permitted under the Collaboration Agreement no part may be reproduced in any form without written permission.
Disclaimer
This document has been prepared in good faith on the basis of information available at the date of publication without any independent verification. The Digital Health & Care Institute (DHI) does not guarantee or warrant the accuracy, reliability, completeness or currency of the information in this publication nor its usefulness in achieving any purpose. Readers are responsible for assessing the relevance and accuracy of the content of this publication. The DHI will not be liable for any loss, damage, cost or expense incurred or arising by reason of any person using or relying on information in this publication.