Ritual Respect
Co-designing care and emotional support around miscarriage
INTRODUCTION
Miscarriage is sadly the most common type of complication associated with early pregnancy, with approximately one in four pregnancies ending in miscarriage. For each woman the experience is different, and access to the right information and emotional support at the right time is crucial to enable them to cope with their loss. However, ongoing emotional support provision for women following miscarriage that meets individual needs is notably lacking, which for many can result in enduring negative effects on their health, relationships, and future pregnancies. This gap in healthcare provision also has wider implications for NHS services, capacity and resources in the long run.
Ritual Respect was led by The Innovation School at The Glasgow School of Art in collaboration with NHS Grampian, and funded by the Digital Health & Care Institute (DHI).
We employed a participatory design approach, collaborating with: women who have experienced miscarriage, health professionals who are involved in providing care around miscarriage (i.e, consultants, midwives and specialist midwives), and representatives from a perinatal counselling group. A series of engagements including Pre-Lab sessions and three Experience Labs were organised over a period of four months.
Analysis and synthesis of the Lab outcomes (i.e, the conversations, maps, artefacts and concept prototypes) offered rich insights around: women’s experiences of miscarriage and scenarios of accessing care; current care pathway capturing key stages and experiences from the perspective of health professionals and women; qualities of preferable care; and concepts for a preferable model of future care by focusing on the emotional care journey.
This webpage presents a summary of the key activities and findings from the project.
project video
Video credit: Hannah Laycock, 2017
methodology
A participatory design approach was used to engage with women who have experienced miscarriage and health professionals who are involved in providing care around miscarriage (i.e, consultants, midwives and specialist midwives) and representatives from a perinatal counselling group.
Image credit: Hannah Laycock, 2017
key FINDINGs
Key findings from the Labs are synthesised into four visual summaries:
Participant’s personal experiences of early pregnancy loss.
Key qualities of care based on key themes emerging from the personal stories of miscarriage shared by the participants.
Map of current experiences of care captured from the perspective of women who have experienced miscarriage and health professionals providing care at different stages of the care pathway.
Concepts and framework for future care focussing on enhancing emotional wellbeing.
Image credit: Hannah Laycock, 2017; Louise Mather 2017
PERSONAL EXPERIENCES
The visuals presented here detail two participant’s personal experiences of pregnancy loss, exploring their circles of care throughout their individual journeys and highlighting the main insights. Pseudonyms have been used to protect the women’s identity.
MAUREEN'S CARE EXPERIENCE
Maureen experienced one miscarriage before she had her daughter, her ‘rainbow baby’. Her experience of bereavement and care over time is represented in the visual below.
Credit: Angela Tulloch, 2018
Before
A lack of information provided by the GP when Maureen presented with symptoms of spotting led to anxiety.
There is a need for upfront, clear information of the eventualities so that women are more prepared in the case of a miscarriage.
During
During diagnosis an absence of appropriate support was hightlighted.
Sometimes family members do not know how to respond to the loss or support the person. There is a need to create more awareness and support people following loss, as well as ensure that health professionals are trained to respond appropriately.
After
The impact on the partner in these situations and negative self-judgement make communicating feelings of grief difficult with the people closest.
Miscarriage can be a natural part of the reproductive cycle yet is seen as a taboo. There is a need to create public awareness to begin to break down barriers.
Long Term
Grief can remain dormant for a long time but is often triggered by certain events.
It is important to have coping mechanisms and a source of comfort and reassurance, a place to mark the loss or positive action.
LINDA'S CARE EXPERIENCE
Linda experienced 10 pregnancy losses including 9 miscarriages and 1 ectopic pregnancy. She had 2 attempts of IVF treatment. She does not have any children. The experiences represented here are the ones that stood out in Linda’s memory.
Credit: Angela Tulloch, 2018
First
A breadth of negative emotions were expressed around this experience, impacting on the ability to process the grief.
The way the loss is communicated to the woman immediately after diagnosis of miscarriage can have a lasting impact on how grief is managed and on future pregnancy experiences.
Worst
This is not a single experience but the build up of multiple bereavements and associated meaning which contributed to the significance of this experience. There were also incidents where a lack of information and communication contributed to anxiety for both her and her partner.
Other life events can cause stress, trauma and anxiety. A person-centred approach to supporting women around miscarriage is needed to provide holistic care.
Most recent
Searching for reasons is a common reaction following miscarriage as having a child can be all they have hoped and dreamt of for the future.
There is a need for information and support for women to make realistic future plans.
qualities of care
The visual presented here brings together the key qualities of care around miscarriage that emerged from the personal experiences of the women who participated in the Labs. The symbols and their meanings were chosen by the women to represent the common links between their individual experiences.
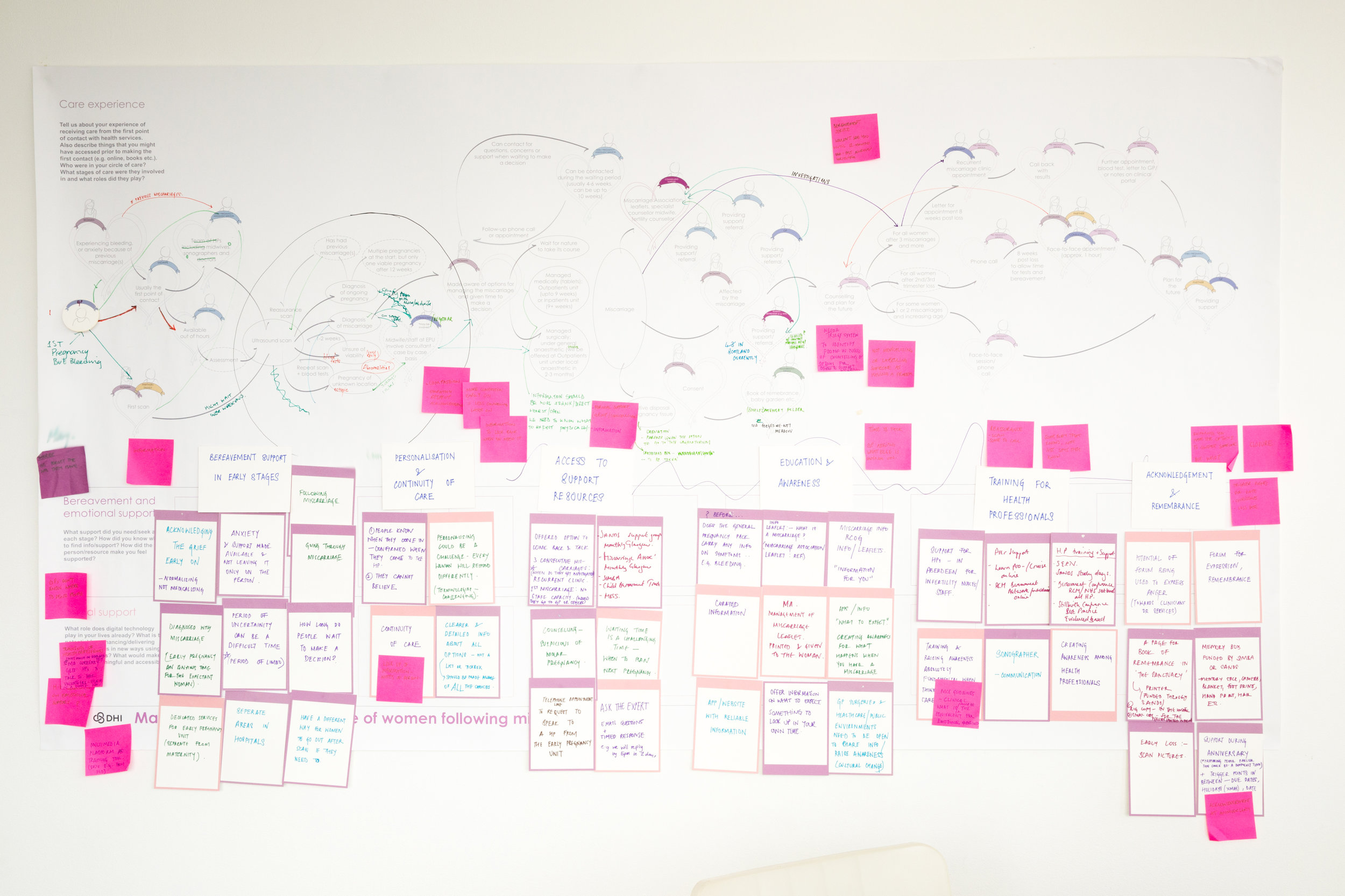
current experience of care around miscarriage
The map captures the various stages of a woman’s journey of accessing care, along with the people, activities and resources involved in each stage. Key moments where there is a gap in current care and opportunities for enhancing support are highlighted along with supporting insights and quotes from the participants.
Credit: Sneha Raman, 2018
Future care around miscarriage: Enabling emotional wellbeing
Credit: Sneha Raman, 2018
Overall insights from the project highlight that each woman’s experience and their way of coping with the loss following miscarraige is unique. A linear care pathway is inadequate for providing care and support that is tailored to each individual. Additionally, current pathways focuses on the stages following the loss and in the later stages of the journey for providing emotional care. The insights from the project, however, emphasises the need to prepare women before and focus on emotional care during the early stages of loss.
Based on these insights, the above visual captures the five key areas focusing on emotional wellbeing in the future:
1. Being prepared: Increasing awareness on early pregnancy loss and training health professionals is key for being prepared and managing expectations.
2. Time and space to grieve: Ensuring early emotional support soon after diagnosis of miscarriage is crucial and sets the tone for the rest of the care journey.
3. Emotional support: Provide health professionals the time and tools to create tailored care plan for the woman, which includes local support and access to information in their own time.
4. Remembrance: Empower women to make personal choices around remembrance and ensure access to physical, digital and symbolic services and platforms.
5. Hope for future: Ensure all women have the freedom to choose support for bereavement, counselling and planning future pregnancies based on personal needs.








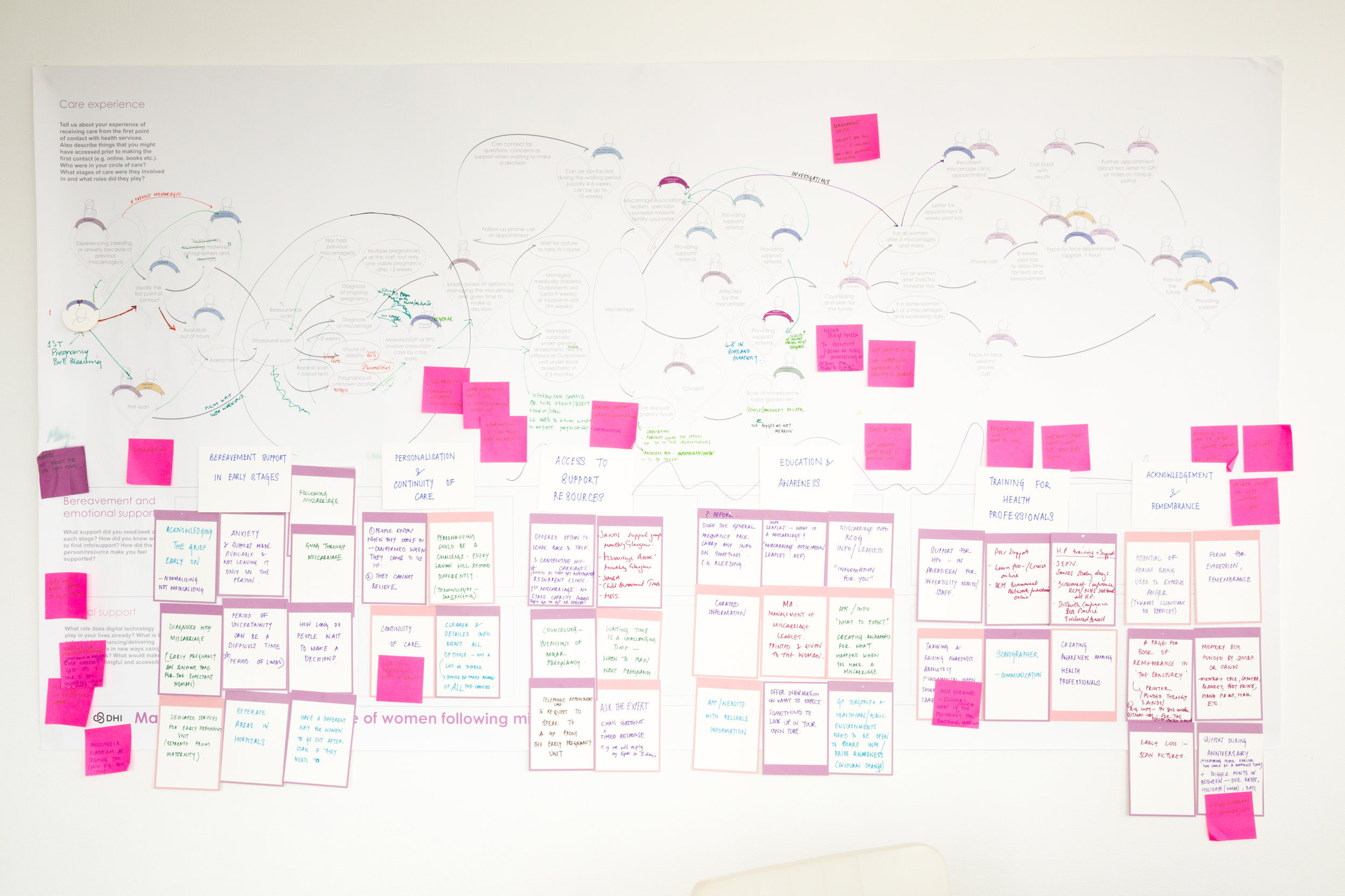


Image credit: Hannah Laycock, 2017; Louise Mather, 2017
next steps
Key actions and opportunities for developing future projects have been highlighted in the final project report, including: auditing bereavement and remembrance services and sharing of good practices standardising information and access to care across Scotland; creating awareness and upskilling the communities through roadshows and training programmes; and creating guidelines for emotional care. These findings were presented to the Scottish Early Pregnancy Network (SEPN).
A number of concepts for the future emphasise the need to create capacity and develop the necessary infrastructure to support the shift from a clinical linear model of care to focus on emotional person-centred care. It is important to address this systemic and cultural shift in order for digital platforms and tools to be able to play a meaningful role in enabling care.
Acknowledgements
We would like to thank our project partner Prof. Grant Cumming, Consultant Obstetrician and Gynaecologist, NHS Grampian, and Prof. Susan Klein, Professor in Trauma Research, Academic Consultant for their inputs and feedback.
We would like to thank all of our participants for giving up their valuable time to take part in the Experience Labs. We would also like to thank Ruth Bender-Atik, National Director of The Miscarriage Association, for her valuable inputs towards reviewing the project plan and recruiting participants. We are grateful for the support of our colleagues at The Glasgow School of Art.
Project OUTPUTS
Project report (web friendly format)
To cite this report: Raman, Sneha and Tulloch, Angela. 2018. Ritual Respect: Co-designing care and emotional support around miscarriage. Project Report. Glasgow School of Art.
Ritual Respect postcards with key quotes from research participants, which was shared publicly during Baby Loss Awareness Week 2017 can be downloaded here:
Postcard 1 | Postcard 2 | Postcard 3 | Postcard 4 | Postcard 5 | Postcard 6 | Postcard 7


















![DHI Full Logo [BLACK].jpg](https://images.squarespace-cdn.com/content/v1/5ab504e77c9327e5eed2778a/1531319867210-M02FPL5598QMMOFTLSKH/DHI+Full+Logo+%5BBLACK%5D.jpg)