Atrial Fibrillation
mapping experience of AF screening in secondary care following stroke
Technology Enabled Atrial Fibrillation Detection after a Stroke in Scotland is a collaborative project with The Glasgow School of Art, NHS Lanarkshire and University of Strathclyde to investigate the current pathway of care for those who have been, or will be, screened for atrial fibrillation (AF) following a stroke. AF is a common abnormal rhythm of the top chambers of the heart which leads to an irregular pulse and is associated with a five-fold risk of stroke. Therefore, detection of AF following a stroke is crucial to prevent recurrent stroke. At present, there is no systematic manner for identification of AF adopted after a stroke in Scotland. Although NICE guidelines recommend at least 72 hour monitoring following stroke to identify the presence of AF, this guidance is not routinely adopted and methods for monitoring are variable nationwide.
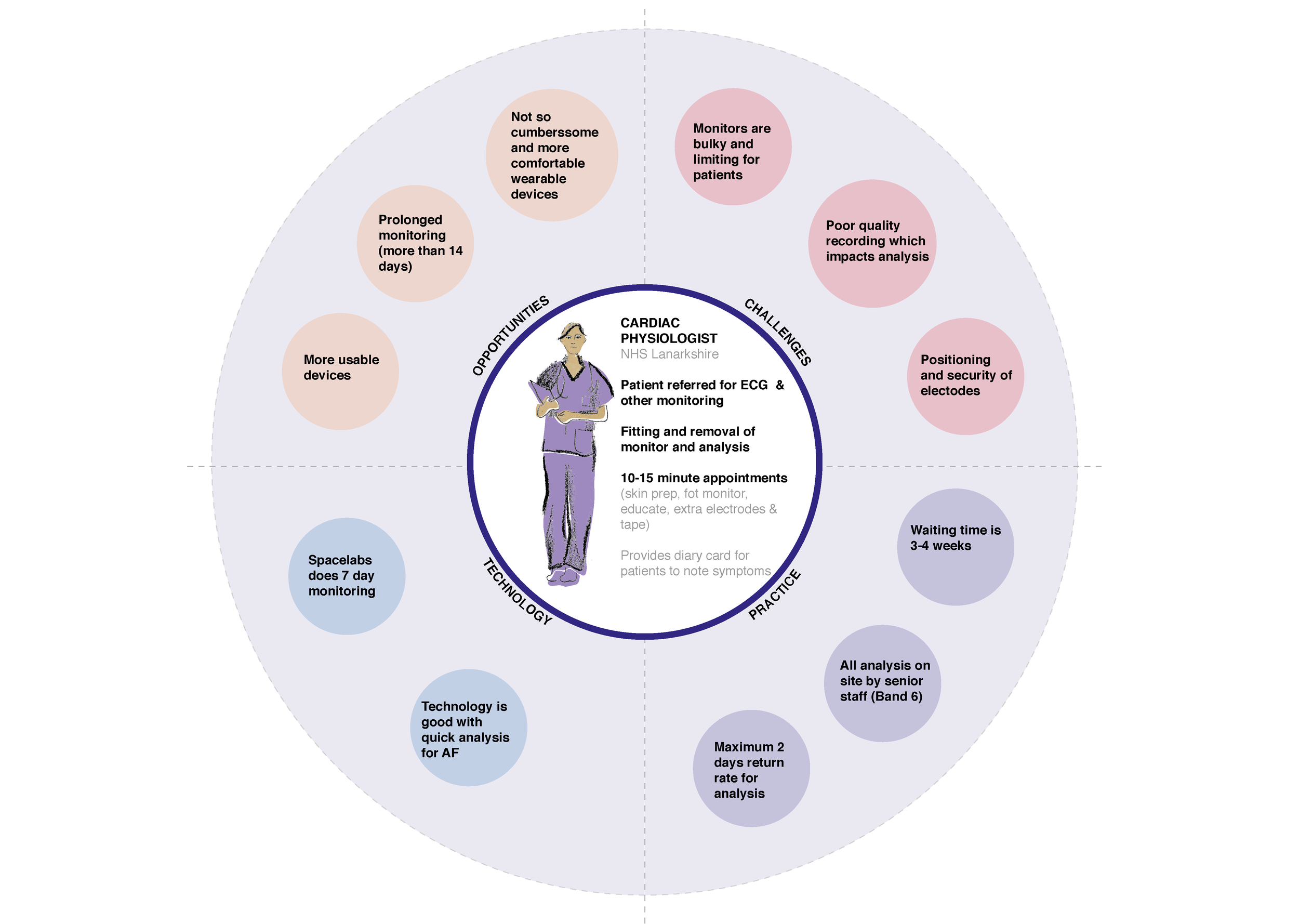
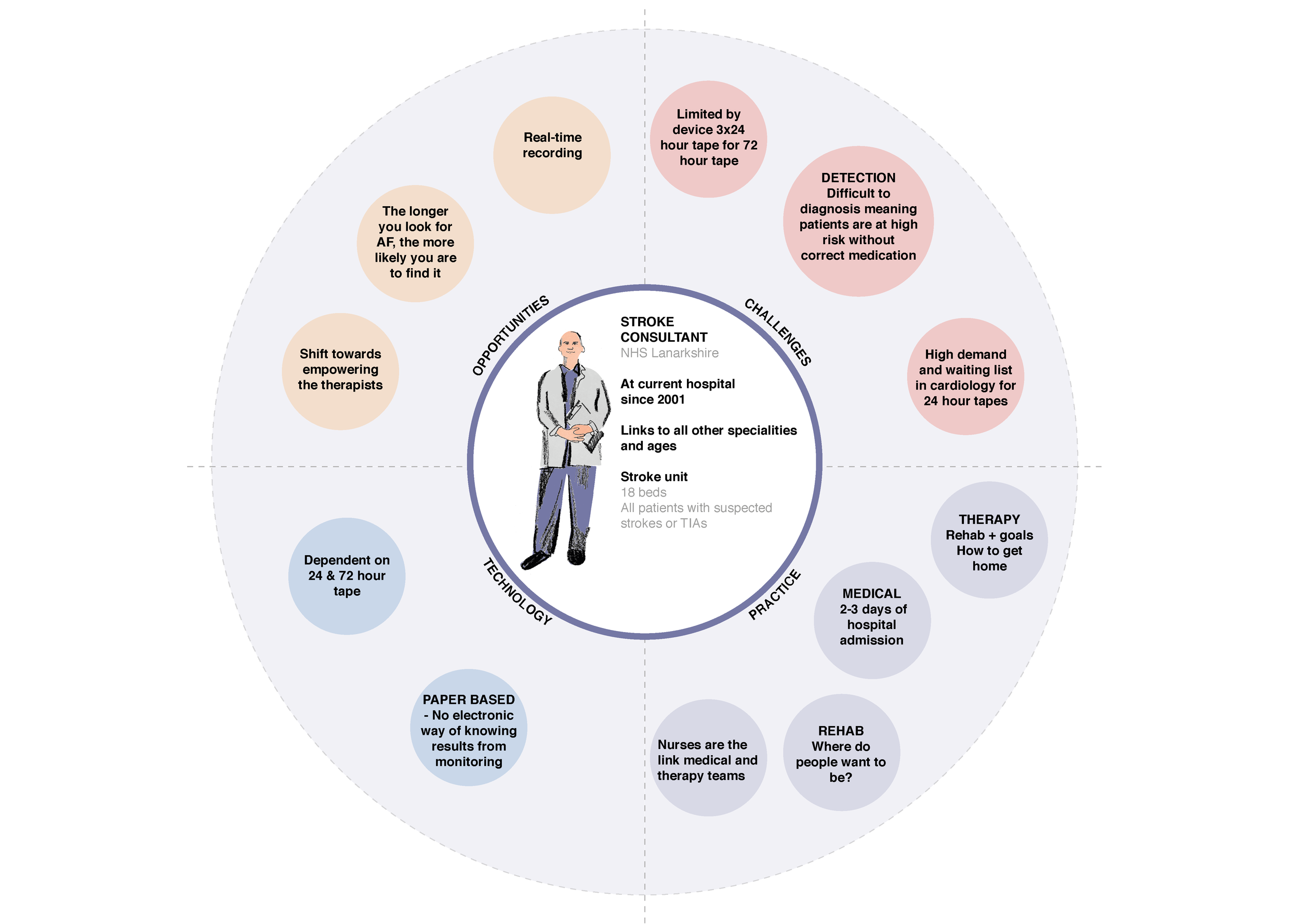
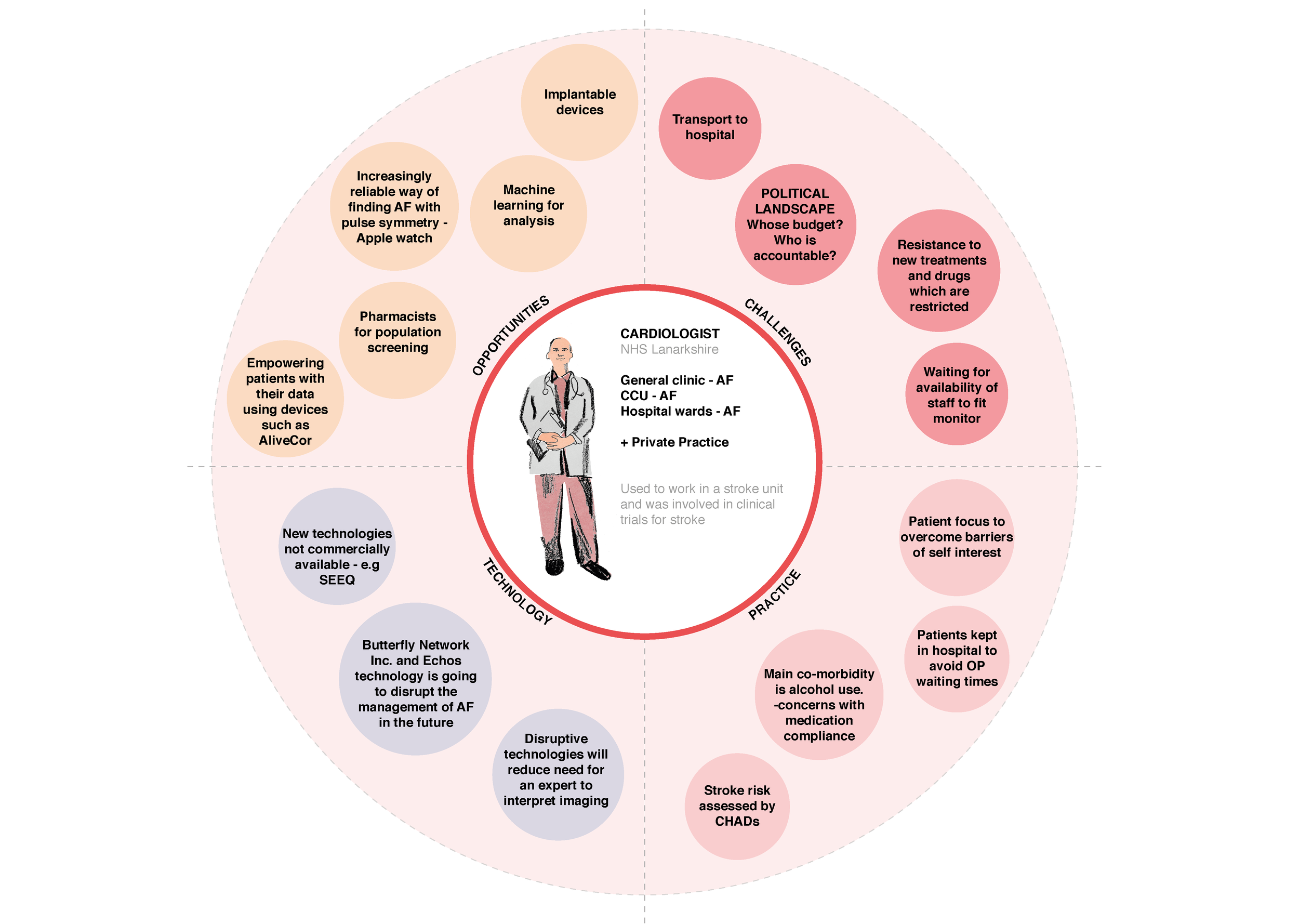
Through employing a participatory design approach including a series of staff and patient interviews using a visual mapping tool, the project aims to understand the current challenges, use of technology and opportunities to innovate in AF services in secondary care. Insights from the study will help academics and health professionals to better understand individual needs and deliver enhanced care in the future.
BACKGROUND
The Technology Enabled Atrial Fibrillation Detection after a Stroke in Scotland project was collaboratively developed by NHS Lanarkshire, subject specialist Professor Lis Neubeck, the University of Strathclyde and The Glasgow School of Art to research AF services in secondary care in NHS Lanarkshire. The enquiry considered the potential of digital technologies in detecting intermittent AF following a stroke, helping reduce the likelihood or reoccurrence of stroke and to support new stroke standards in an efficient and effective way.
AF is a common abnormal rhythm of the top chamber of the heart which leads to an irregular pulse and is associated with a five-fold risk of stroke. AF can affect adults of any age, but it becomes more common as you get older, affecting about 7 in 100 people aged 65 and over and more prominently with men than women (NHS, 2015). In Scotland, it affects an estimated 96,000 people and it is estimated that as many as one third of people with AF are undiagnosed and therefore at risk of having a stroke (British Heart Foundation, 2018). In general, the strokes associated with AF are more severe and are therefore more likely to lead to hospital admission, death or long-term disability can have a devastating impact on survivors’ lives, and that of their family and loved ones as well as leading to high care costs (British Heart Foundation, 2018; Neubeck, L et al, 2017). To add further complexity, episodes of AF can be intermittent and often don’t present with symptoms making identifying the condition challenging. Following a stroke, to more effectively identify AF in some individuals, longer screening periods may be required (Kirchhof et al., 2016).
Currently, there is no systematic manner for identification of intermittent AF following a stroke adopted across primary or secondary care in Scotland. Although the ESC (European Society of Cardiology) guidelines (Kirchhof et al., 2016) recommend a minimum 72 hour monitoring following stroke to identify the presence of AF (NICE, 2014), this guidance is not adopted uniformly and methods for monitoring are variable nationwide. New standards have also been agreed by the National Advisory Committee for Stroke which should enhance the detection of AF in those who have had an ischaemic stroke or transient ischaemic attack (TIA).
In Scotland the standard method for detecting AF following a stroke or TIA is usually by a 12-lead ECG, and may also be augmented by in-patient telemetry. A 12 lead ECG captures a 30 second snapshot of the electrical rhythm of the heart however, this may not detect intermittent episodes of AF. If there is a high suspicion that the origin of the stroke or TIA is cardiac, then longer term monitoring may be warranted. Current prolonged monitoring involves Holter ambulatory monitor method using a small battery powered device. This equipment needs to be fitted and removed by staff in an outpatient setting. The timeframe within which results are analysed and reported differs from one hospital to another but currently the majority of health boards across Scotland struggle to deliver prolonged monitoring with results available within 2 weeks.
A cross-party inquiry led by the British Heart Foundation recommended investments in the use of proven technologies within clinical practice to detect AF and work with stakeholders in primary and secondary care to create a clear and consistent clinical pathway for people diagnosed with AF (British Heart Foundation, 2018). Therefore improved detection, diagnosis and appropriate treatment of AF present an opportunity to reduce the impact of stroke in Scotland.
The value of collaboration across the health sector is well documented and coproduction and co-creation are core principles embedded within the NHS. It is accepted that the inclusion of end-users is crucial to the success of the innovation in order to ensure that the needs and preferences of end-users are met in the developed solution. (Kline, S. et al., 1986).
Further to this, recognising that co-created, iterative methodologies using designers and a 'bottom up' approach have the potential to develop more person-centred service innovation (Bate, P. 2004, 2006), this project therefore seeks to gather insight from key health professionals to promote and support a recommended practice in a cost effective and efficient way that will contribute to a person-centred care pathway.
Approach
Design has an important role to play in addressing complex and challenging contexts across health and care. Using collaborative and participatory methodologies, design can provide explorative and speculative approaches to begin to unpick both tangible and intangible issues and translate these into opportunities for change. In this way, design can meaningfully enable the reconfiguration of services, products and processes, responding to the needs and aspirations of all stakeholders involved and capitalising on new insights to support transformation.
Within the AF project, the engagement of stakeholders was a central component of the planned design activity. It is recognised that in order to identify possible futures for AF care, it is critical to first explore and understand the current context, validating challenges and opportunities identified and generating a rich resource of multiple perspectives upon which to test, refine and demonstrate possible new futures.
This service evaluation project is part of a larger research project lead by the University of Strathclyde. The overall purpose of this project was to identify and utilise digital technologies to help reduce the reoccurrence of stroke and to support new stroke standards in an efficient and effective way. The aim of which was to gather user experiences, expectations and positive and negative reactions to (i) the current AF service pathway, (ii) the new AF device(s) being considered and (iii) the potential future AF service as new devices for detecting AF are rolled out. Unlike many other health studies – this research focuses on user experiences and expectations rather than health outcomes.
The aim of this service evaluation work was to investigate the current pathway of care for those who have had an ischaemic stroke or transient ischaemic attack (TIA) and have been monitored for the presence of AF in order to understand the current challenges, use of technology and opportunities to innovate AF services in secondary care, from the perspectives of NHS Lanarkshire staff involved in delivering that care. The design activity (in particular, the interviews around the current state) contributes towards the development of an interactive, evidence-based demonstration of future AF care, enabled by digital technology.
Please note that due to some set backs and time constraints with the project, no patient interviews were completed as part of this phase of the work and therefore not represented in the subsequent findings.
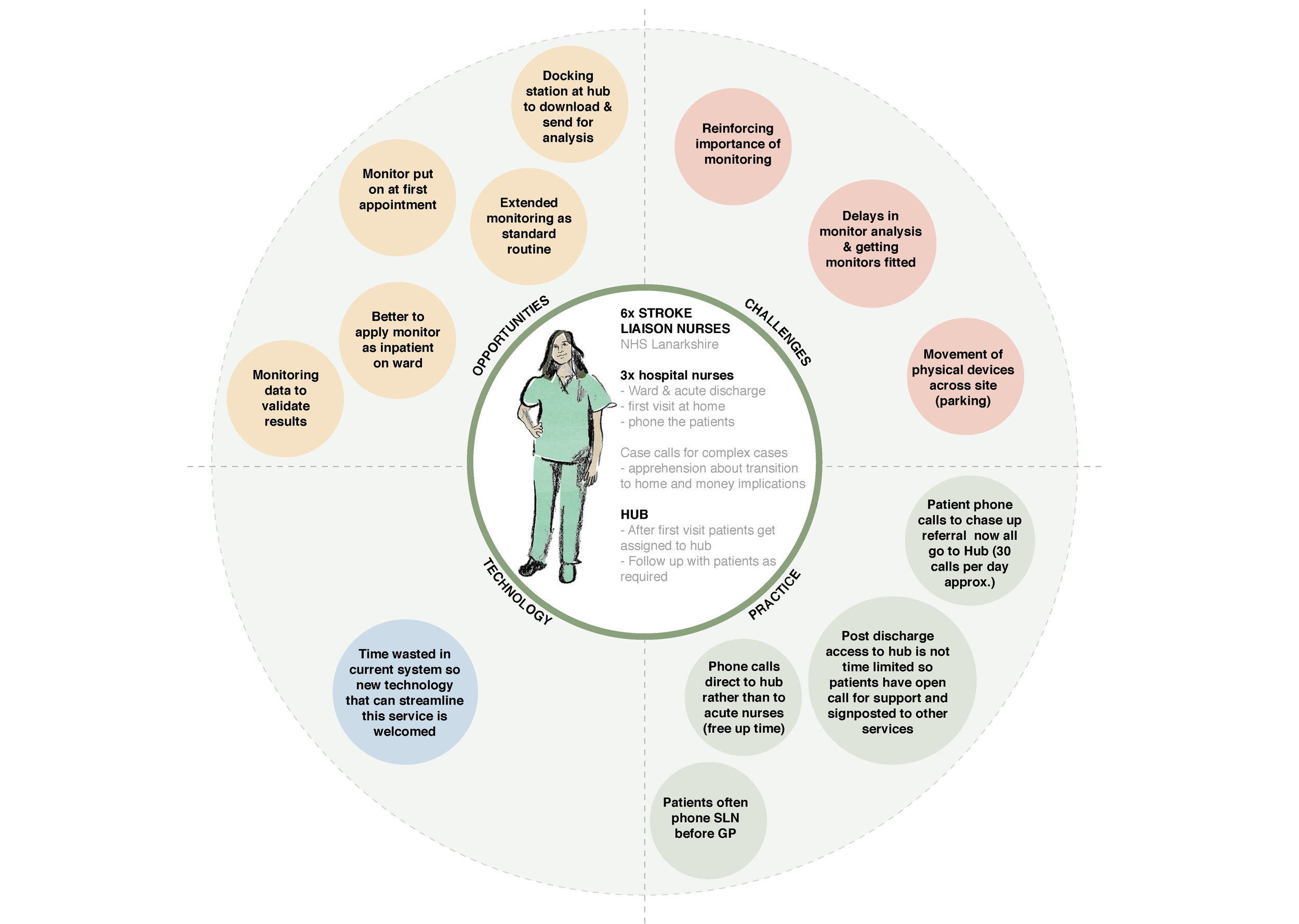
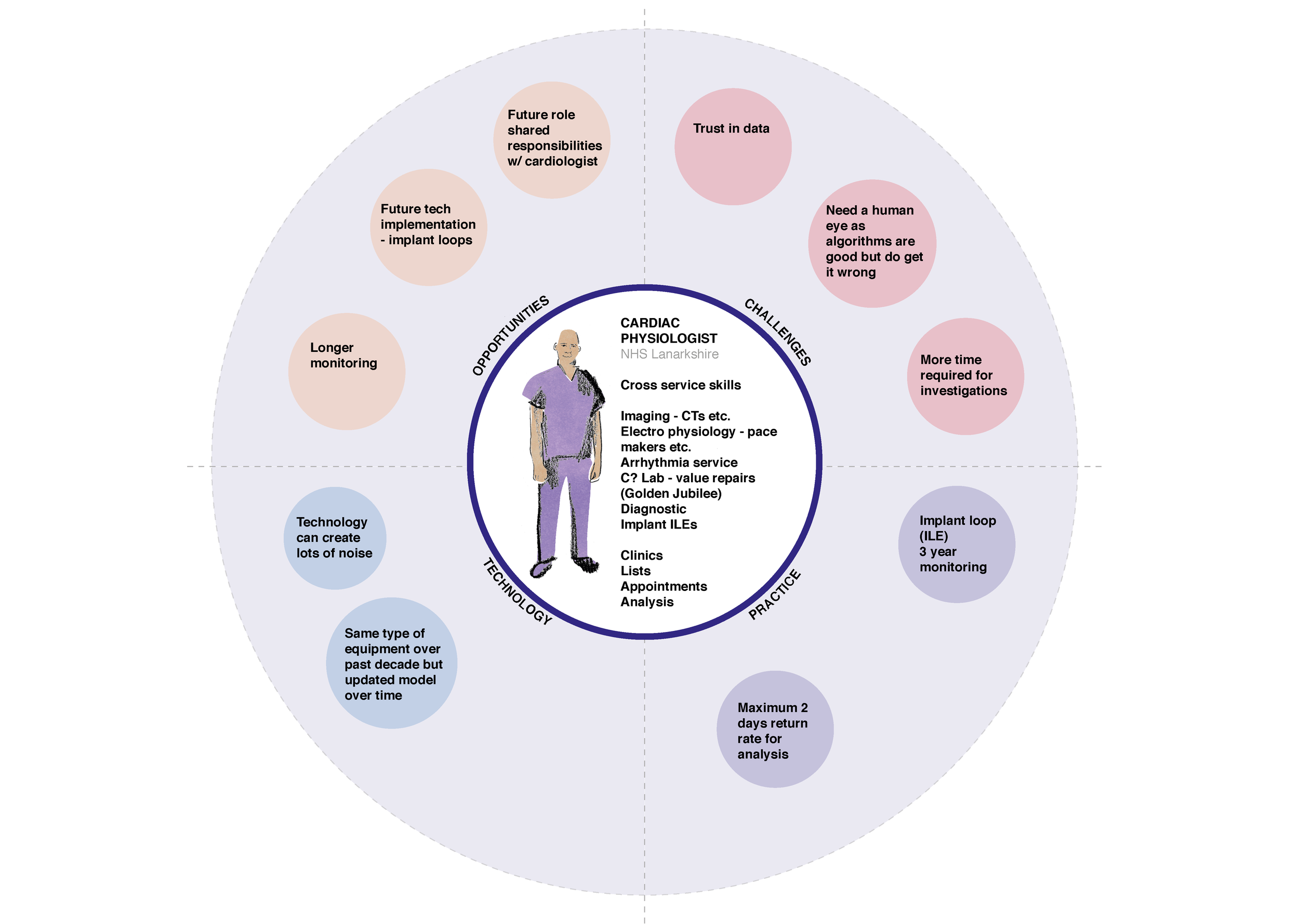
CURRENT STATE MAP: HEALTH CARE PROFESSIONALS
The current clinical pathway presented below has been distilled from 10 interviews with NHS Lanarkshire staff including a Cardiologist, Stroke Consultant, Nurses and Clinical Physiologists. The interactive pathway allows you to explore the patient journey through insights gathered as well as challenges and opportunities identified. There is also the option of an overview which collates the service challenges and opportunities together and is available as a downloadable version.
The outputs of the current state mapping were fed into further work led by the University of Strathclyde to investigate AF detection services in secondary care in NHS Lanarkshire and to evaluate the use of a new technology supported AF service and secondary care pathway in NHS Lanarkshire (to understand how this might scale nationally).
health care professional roles
REFERENCES
Bate, P., Robert, G. and Bevan, H. (2004). The next phase of healthcare improvement: what can we learn from social movements?. Quality and Safety in Health Care, 13(1), pp.62-66.
Bate, P. and Robert, G. (2006). Experience Based Design: from redesigning the system around the patient to co-designing services with the patient. Quality and Safety in Health Care, 15(1), pp.307-310
British Heart Foundation (2018) Focus on Atrial Fibrillation in Scotland: a report by the Cross-Party Group on Heart Disease and Stroke, available from <https://www.bhf.org.uk/get-involved/heart-voices/updates-on-our-current-projects/cross-party-group-inquiry-into-atrial-fibrillation-in-scotland > accessed 23/01/18
Braun, V., and Clarke, V. (2006). Using thematic analysis in psychology, Qualitative Research in Psychology. 3(2), 77-101
Cornwall, A. and Jewkes, R., 1995. What is participatory research?. Social science & medicine, 41(12), pp.1667-1676.
Kirchhof, P., Stefano Benussi, S., Kotecha, D, Ahlsson, A., Atar, D, Casadei, B., Castella, M., Diener, H., Heidbuchel, H., Hendriks, J., Hindricks, G., Manolis, A.S., Oldgren, J., Popescu, B.A., Schotten, U., Van Putte, B., Vardas, P., ESC Scientific Document Group; (2016) ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS, , European Heart Journal, 37(38), pp.2893–2962, available from < https://doi.org/10.1093/eurheartj/ehw210> accessed 23/01/18
Kline, S. and Rosenburg, N. (1986). An overview of innovation. In Landau, R., and Rosenberg, N., (eds.), The Positive Sum Strategy: Harnessing Technology for Economic Growth. Washington, D.C.: National Academy Press.
Neubeck, L., Orchard, J., Lowres, N., & Freedman, B. (2017). To screen or not to screen? Examining the arguments against screening for atrial fibrillation. Heart, Lung and Circulation, 26(9), (880-886). doi:10.1016/j.hlc.2017.05.118. ISSN 1443-9506
National Health Service (2015) https://www.nhs.uk/conditions/atrial-fibrillation/ - accessed 13/12/17
NICE (2014) Atrial Fibrillation: management, available from <https://www.nice.org.uk/guidance/cg180> accessed 13/12/17
Project TEAM
Angela Bruce (a.bruce@gsa.ac.uk) - Research Associate, Glasgow School of Art
Dr Marilyn Lennon - Senior Lecturer, University of Strathclyde
Dr Lisa Macann - Senior Lecturer, University of Strathclyde
Sarah Horan - Research Assistant, University of Strathclyde
Professor Mark Barber - Stroke Clinician, NHS Lanarkshire
Katrina Brennan - Stroke MCN Manager, NHS Lanarkshire
Professor Lis Neubeck- Head of Cardiovascular Health, Edinburgh Napier University
Copyright
This publication is copyright. Apart from any use as permitted under the Collaboration Agreement no part may be reproduced in any form without written permission.
Disclaimer
This document has been prepared in good faith on the basis of information available at the date of publication without any independent verification. The Digital Health & Care Institute (DHI) does not guarantee or warrant the accuracy, reliability, completeness or currency of the information in this publication nor its usefulness in achieving any purpose. Readers are responsible for assessing the relevance and accuracy of the content of this publication. The DHI will not be liable for any loss, damage, cost or expense incurred or arising by reason of any person using or relying on information in this publication.