Redesigning the care journey for
people living with functional disorder
IN PARTNERSHIP WITH NHS GRAMPIAN
INTRODUCTION
This project is a collaboration between The Glasgow School of Art (GSA), NHS Grampian and Robert Gordon University (RGU). It sought to identify opportunities and develop new ideas to shape how people living with functional disorder are supported in NHS Grampian. It was initiated and funded by NHS Grampian, commencing in May 2020 and completing December 2022.
METHODOLOGY
Scoping review
The project started with a scoping review on ‘Management of Functional Disorders’ undertaken by researchers at Robert Gordon University, led by Professor Kay Cooper. This mapped the existing evidence base for the management of functional neurological disorder (FND), fibromyalgia, and irritable bowel syndrome (IBS). The review aimed to provide an overview of the available literature on: i) reported pathways for patient management, and ii) reported treatments/interventions.
Interviews with people living with functional disorder
Meanwhile, design researchers at the Innovation School at GSA undertook scoping interviews with a small number of clinicians from primary and secondary care. The aim of these sessions was to gain understanding of the context to inform the design of interviews with people living with functional disorder. As a result, a bespoke experience mapping tool was designed to structure the interviews and record interviewees’ experiences.
The aim of the interviews was to generate rich accounts of the service/pathway from the perspectives of people living with functional disorder and who access related services in Grampian, to understand what works and what needs to be improved. The aim of the experience maps was for the health professionals to see and understand how patients make sense of their experience, and what impact aspects of care have on their attitude and behaviours (e.g. their willingness and ability to engage in self management). In addition, the care pathway for functional disorder is often very fragmented and can involve patients ‘going round the houses’ and seeing a number of different specialists on their journey to a diagnosis. Health professionals currently only see discrete parts of the journey (from their own perspective/part of the system of care), and the experience maps show the individuals’ journeys in their entirety helping them to understand the whole journey from the perspective of those receiving care.
We aimed to conduct nine interviews – three each with people living with Fibromyalgia, IBS and FND. Recruitment for IBS and FND fulfilled the required numbers, however, only two participants volunteered for Fibromyalgia. Thus, eight interviews were completed in total.
Condition specific co-design workshops with health professionals
Following the lived experience interviews for each condition, three condition specific workshops were organised with health professionals currently supporting people living with each condition. The aim was to co-design the ideal pathway for a person living with that condition by responding to the in-depth journeys of people with lived experience and the evidence of effective treatments and pathways gathered by the scoping review.
Activities in each workshop focused on: understanding the different professionals involved and their roles in providing care for people with the specific condition (i.e. FND/ fibromyalgia / IBS); capturing key challenges for health professionals when working with people with the condition; and reviewing the experience maps of people living with the condition alongside evidence relevant to that condition from the scoping review (summarised visually); to inspire and inform the development of a new pathway for that condition.
Overall co-design workshop for Functional Disorder with health professionals
A final in-person workshop brought together health professionals working across the different conditions and services. It aimed to review emerging outputs from the three condition-specific sessions; identify commonalities and differences across the pathways and model(s) of care for people with different functional disorders, and redesign the future experiences of diagnosis and care for people living with functional disorders in NHS Grampian.
Key activities in the final workshops focused on:
reviewing a mixed set of experience maps of people living with FND, fibromyalgia and IBS and capturing commonalities and differences in their needs and experiences by working in two multi-disciplinary groups;
working individually to identify ‘key ingredients’ for a new functional disorders pathway by reviewing ideas and ‘how might we?’ questions on opportunities emerging from the condition specific workshops, alongside ideas for good practice identified in the scoping review;
and working in two breakout groups to collaboratively develop a new combined pathway for functional disorders.
At the end of the workshop all participants worked together to discuss the short to long-term actions required to implement these new pathways, including other departments or people who may need to be involved.
CONDITION SPECIFIC FINDINGS
To view a summary of findings specific to each condition, please follow the links below:
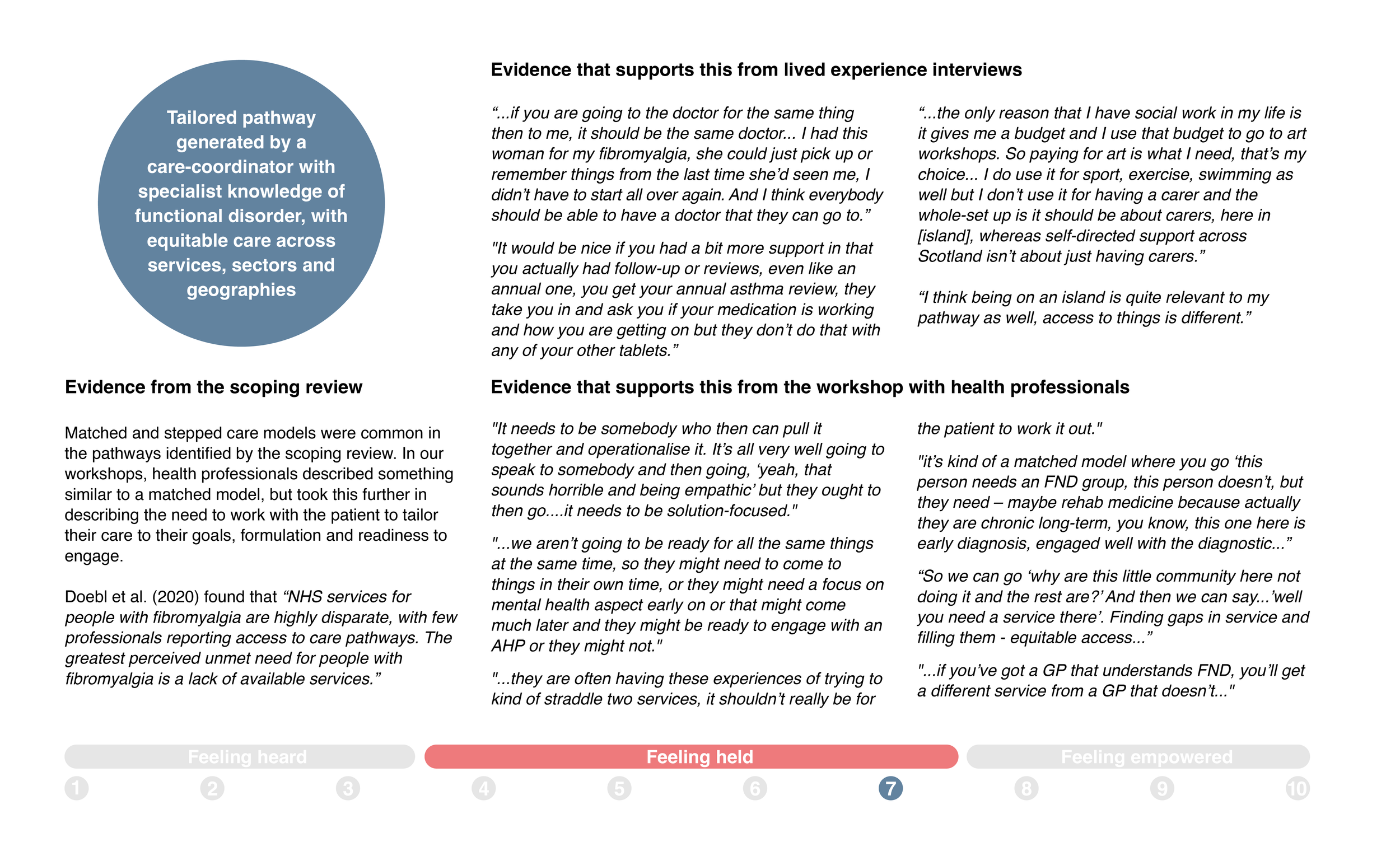
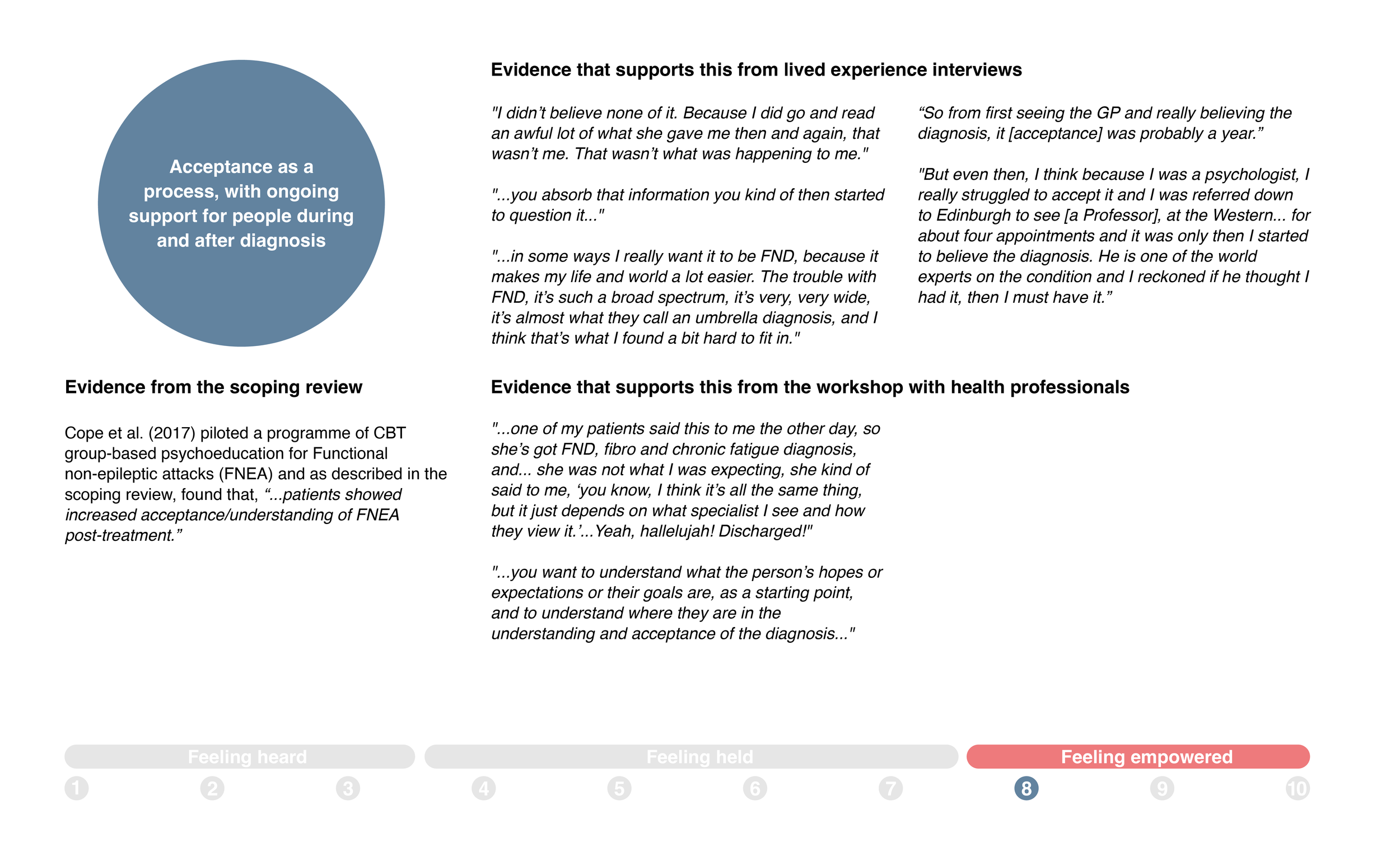
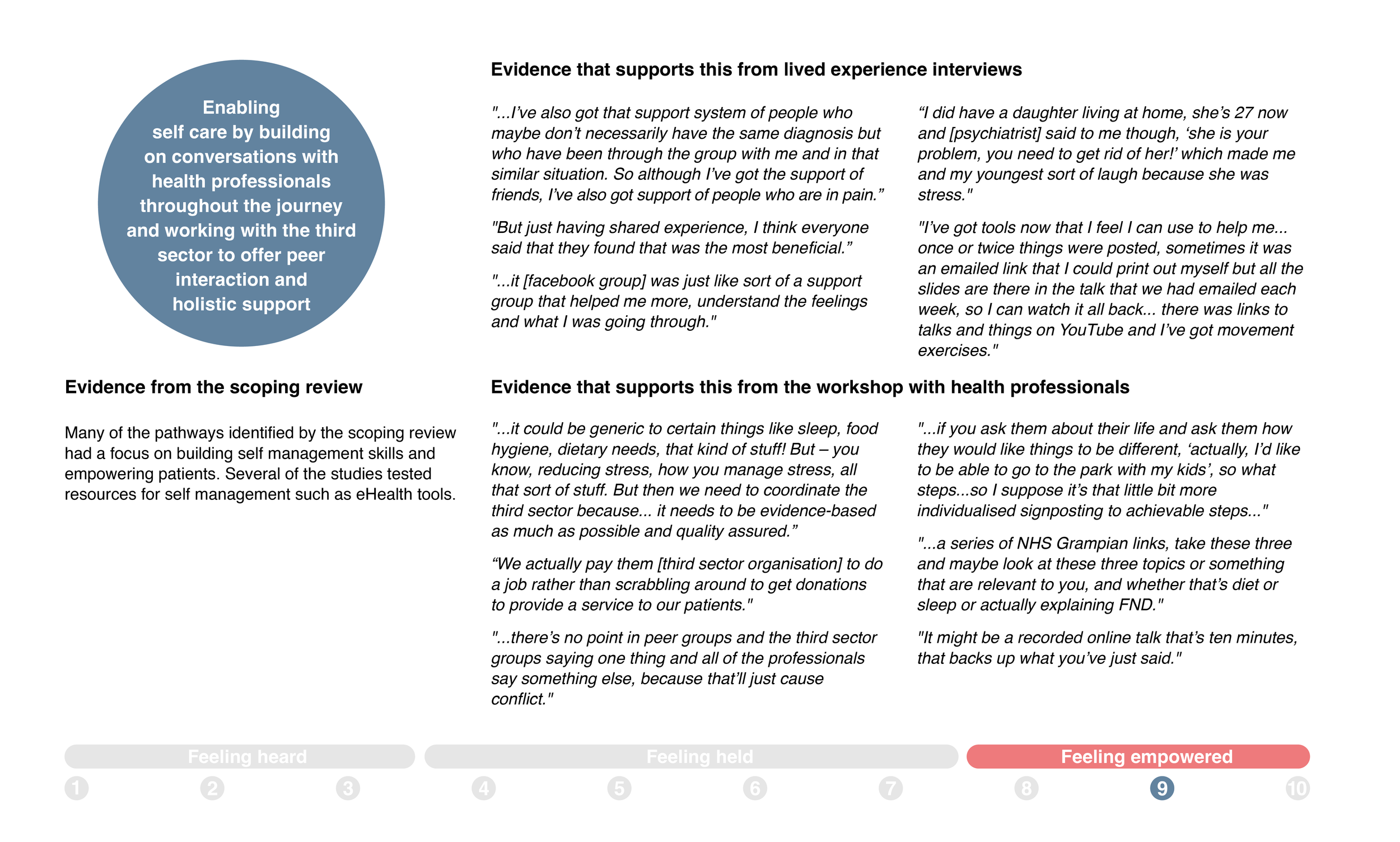
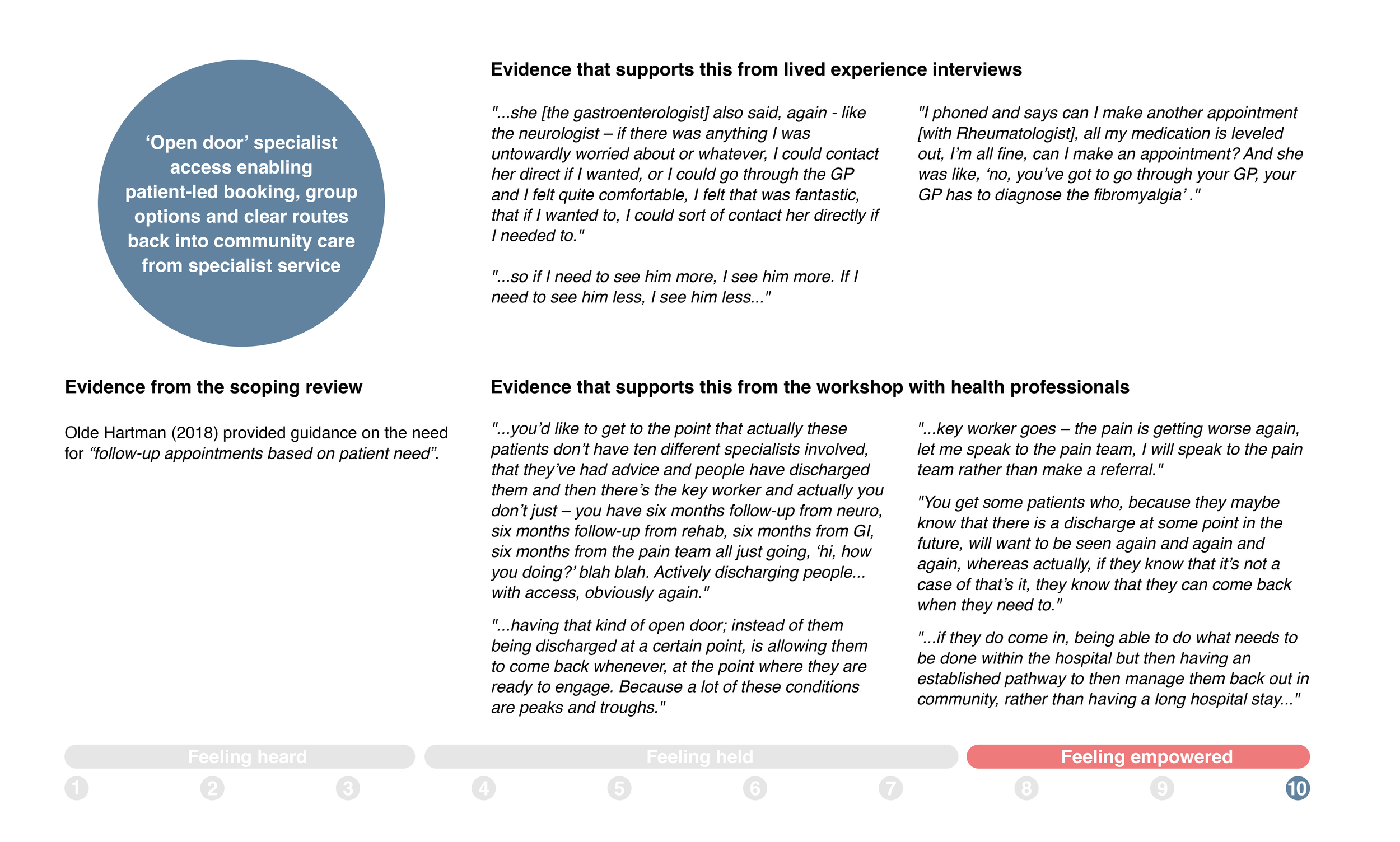
FUTURE PATHWAY FOR FUNCTIONAL DISORDERS
Synthesising the insights from the interviews with people living with a functional disorder and the co-design workshops with health professionals providing care for them, we have proposed a future pathway for functional disorder, which is non-linear and can be tailored to respond to the unique experiences and needs of each individual. Moving beyond a clinical view of service pathways which focus on steps for treatment and management of a condition pre-, during and post diagnosis from a delivery perspective, the future pathway is modelled from the perspective of people living with functional disorders focusing on key stages of their care journey and experience: feeling heard, feeling held and feeling empowered.
Participants in the final co-design workshop also identified two key principles that cut across and guide new ways of working for health professionals to support the person’s journey along the future pathway: building a relationship with the person, and ensuring psychologically informed care for all.
Figure 1: Future pathway modelled around what matters to the person
This section presents an overview of the key principles, followed by an introduction to the three stages of the future pathway. Note that all participant quotes are attributed to their chosen pseudonyms.
KEY PRINCIPLES
Building a relationship with the person
Building a relationship with the person underpins all three stages of feeling heard, feeling held, and feeling empowered, reflecting both the aim of the future pathway as well as how the future pathway could be realised in practice. Building trust and relationships was one of the shared themes that emerged from the experience maps across all three conditions. For example, Luap reflected on a lack of personal touch in his interactions with the NHS and Linda noted that having a connection and building trust with all the people who are involved in her care is important to her.
Psychologically-informed care for all
Adopting psychologically-informed care for all will ensure a more integrated biopsychosocial approach to care across all stages of the future pathway and help to address stigma associated with functional disorders. All health and care professionals involved in caring for people living with a functional disorder receiving training and building skills in psychologically-informed care practices will address current challenges around accessing specialist support and improved quality of care for everyone. Stigma and a lack of focus beyond physical health was a shared theme that emerged from the experience maps across all three conditions. For example –
Luap reflected that in his experience the focus was never on the psychological aspects of his condition, and that psychological support was only available to people in extreme scenarios, and William felt that the focus on stress as a main cause for his condition was stigmatising and lacked evidence.
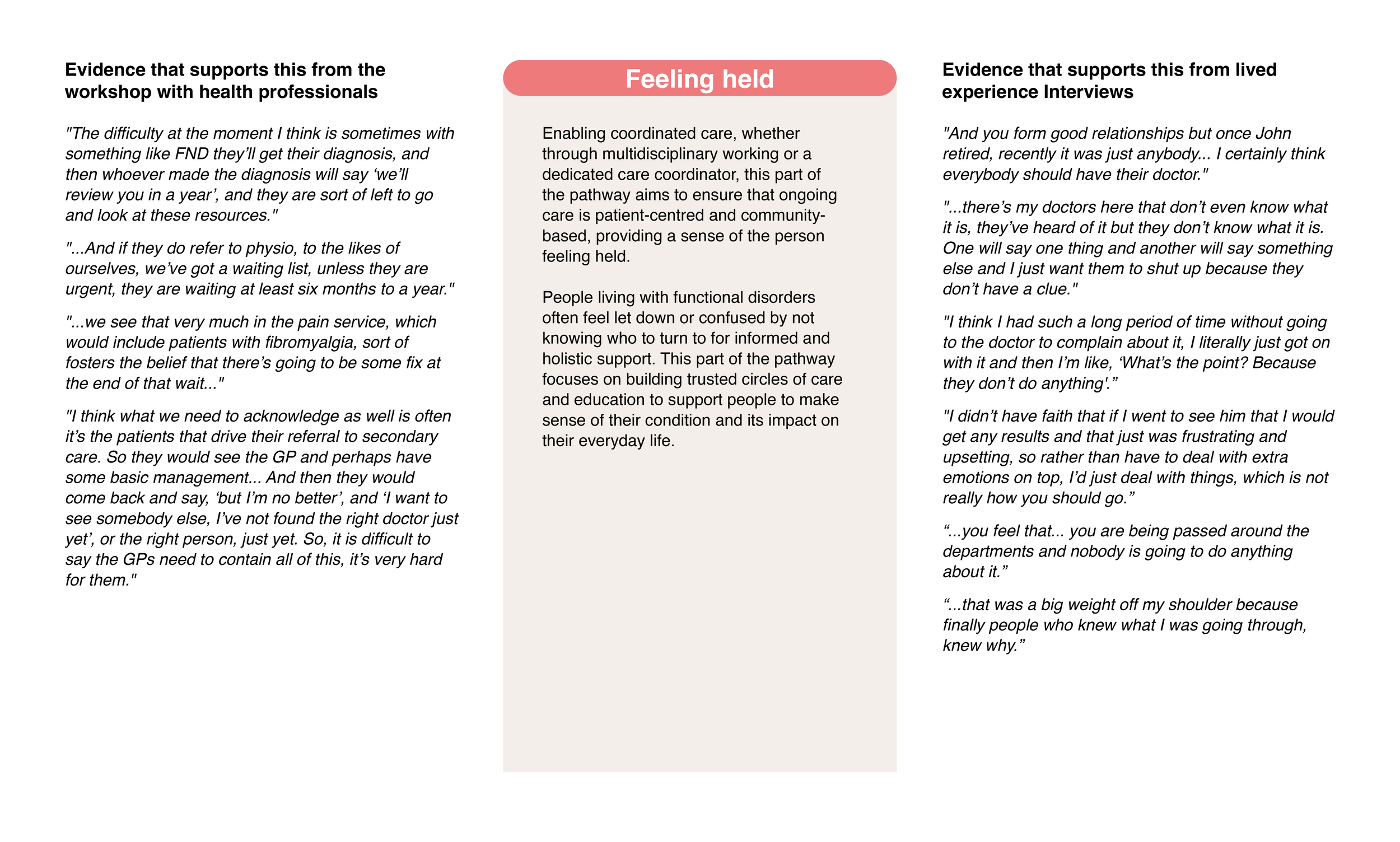
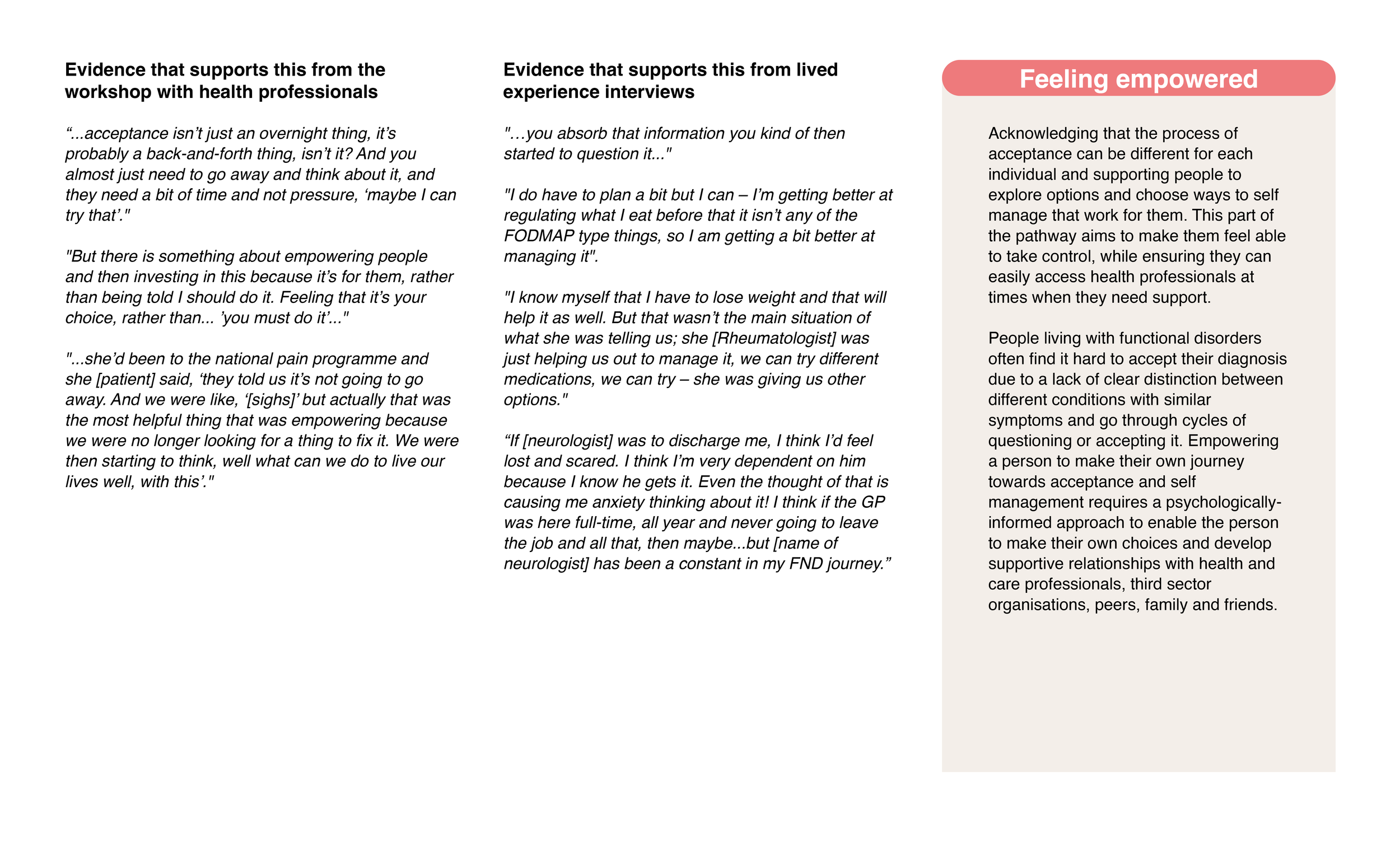
KEY STAGES OF THE FUTURE PATHWAY
The key stages guiding the future pathway – ‘feeling heard’, ‘feeling held’ and ‘feeling empowered’ are described below.
Supporting evidence for each of the three stage is presented below. Please use the arrow keys to review these.

OVERALL PATHWAY
The following visual presents an overview of the proposed future pathway for functional disorders in Grampian.
Supporting evidence for each step in the pathway is presented below. Please use the arrow keys to review these.



The following visual presents a synthesis of the tools and resources required for supporting the implementation of the new pathway.
ROADMAP/NEXT STEPS FOR NHS GRAMPIAN
During the final workshop, participants discussed short- and long-term actions required for implementing a new pathway and potential challenges that need to be addressed.
Participants noted that some of the emerging ideas, such as creating web resources for FND, could be started in the short term. However there are not enough staff to implement others such as ‘open door’ patient-led appointments, which will require longer-term planning.
In this section, we discuss three key areas of focus for implementing the new pathway.
Building leadership
A key focus of this discussion was around building focused clinical and managerial leadership and securing capital investment to guide implementation. Participants agreed that presenting the findings and future pathway emerging from this work to the leadership team in NHS Grampian and identifying the top three priorities should be the first step towards this. Participants agreed that these need to be supported with evidence from research and evaluation. However, participants cautioned that there is a need to build on what we already have before gathering further evidence.
Implementing care coordinators
It was noted that currently, there is a funding bid for a FND practitioner. There is an opportunity to build on learning from this and explore how similar new roles might be created to work across multiple functional disorders.
Participants noted that these roles would be similar to the current MND specialist roles. However, capacity was identified as a potential challenge for functional disorders.
An increasing number of people are currently living with/ newly diagnosed with functional disorders, which could result in large caseloads for care coordinators. Participants recommended that this could be addressed by focusing on providing care coordinators for the most complex cases, while wider community-based services (all trained in psychologically-informed care in the future) could be involved in supporting others.
Ensuring equity
Participants strongly agreed that current variation in management structures and care practices across areas and partnerships is a crucial challenge, and ensuring equity needs to be the main focus at a strategic and managerial level when implementing the new pathway. Participants also felt that there is a danger of things getting stuck at the ‘test of change’ stage.
Participants highlighted that it is difficult to get consistency in care when there is variation in the ways GPs work, so there is a need to involve them in future discussions. Similarly, participants noted a need to involve mental health teams in future discussions to understand where they fit in the pathway to address challenges around patients being sent back following a referral. Therefore there is a need to create a shared understanding across services.
ACKNOWLEDGMENTS
We would like to thank all of our interview participants for their valuable time and for generously sharing their stories to inspire service redesign. We would also like to thank health professionals for their valuable contribution and ideas for future pathways in the co-design workshops.
FUNDING
The project was funded by NHS Grampian, who commissioned The Glasgow School of Art to undertake this research to support their service improvement activities.
PROJECT TEAM
The Glasgow School of Art
Sneha Raman
Angela Bruce
Gemma Teal
Silvia Cantalupi
NHS Grampian
Fiona Summers, Consultant Clinical Neuropsychologist
VISUALS FOR DOWNLOAD
Visual summary of the scoping review evidence
Interview maps:
Elaine (FND)
William (FND)
Linda (FND)
Luap (IBS)
Tess (IBS)
Cat Lady (IBS)
Lily (Fibromyalgia)
Annie (Fibromyalgia)
Key Stages of the Future Pathway with Evidence Cards
Authored by Sneha Raman, Gemma Teal and Silvia Cantalupi, Dec 2022.
FURTHER INFORMATION
For more information about this project please contact:
Sneha Raman, s.raman@gsa.ac.uk
Gemma Teal, g.teal@gsa.ac.uk