MIDLOTHIAN TEC PATHFINDER
TRANSFORMING THE FRAILTY SYSTEM OF CARE
Project video by Louise Mather
Background
Midlothian Health and Social Care Partnership (MHSCP) are forging a path to change frailty identification and management. The journey began by using existing Primary Care records to stratify the population in Midlothian using the eFrailty Index (eFI), and this has led to new insights concerning the scale of the challenge of supporting citizens identified as living with frailty. Through innovative partnerships with the British Red Cross and VOCAL, new ways of supporting people living with frailty and carers were developed, which help people to navigate the system and access support to live well. Alongside this, MHSCP has developed new ways for health, care and third-sector professionals to collaborate and work in multidisciplinary ways to identify people at risk and prevent crises.
To push forward on this path of innovation, MHSCP successfully applied to the Technology Enabled Care (TEC) Pathfinder programme at the Scottish Government for a project exploring how digital technology and design can act as transformation enablers. To date, efforts to provide integrated and patient-centred care across disciplinary and sectoral boundaries have been hindered, rather than enabled, by technology. There is no means of integrating effort and information across our care system – including statutory, third-sector, and citizen-held domains. This lack of integration and data sharing impacts the experiences of people living with frailty and their informal circles of care.
MHSCP partnered with the Digital Health and Care Innovation Centre (DHI) to help them use design-led approaches to engage with citizens and stakeholders and involve them in innovating the frailty care system. The project benefited from strong clinician involvement, a range of key partners, including the British Red Cross and VOCAL, and robust senior management support.
Project Aims
The aims of the project were to:
Improve the experience of people living with frailty, their family and carers, and staff;
Develop safe and highly reliable systems and pathways of care processes;
Breakdown the structural barriers between the organisations within the partnership;
Achieve this in a way that starts with scale in mind.
APPROACH
The TEC Pathfinder programme required that all funded projects follow the Scottish Approach to Service Design. This aims to ensure that the people of Scotland are supported and empowered to actively participate in the definition, design and delivery of their public services. As partners in the DHI, the School of Innovation and Technology at The Glasgow School of Art enabled active participation using specialist expertise in participatory design approaches to creatively engage stakeholders in reimagining the frailty care system. Working collaboratively with DHI colleagues at the University of Strathclyde, we realise new ideas by iteratively prototyping digital products and services with stakeholders, demonstrating and simulating how these new ways of working can transform care experiences.
Stage 1 - Discover & Define
Within this project, we have used a range of bespoke engagements to bring different stakeholder groups into the design process. We needed to understand the current system of care from these different perspectives. We also wished to engage with older people more widely to understand how we can take a preventative approach to frailty and support self management of ageing.
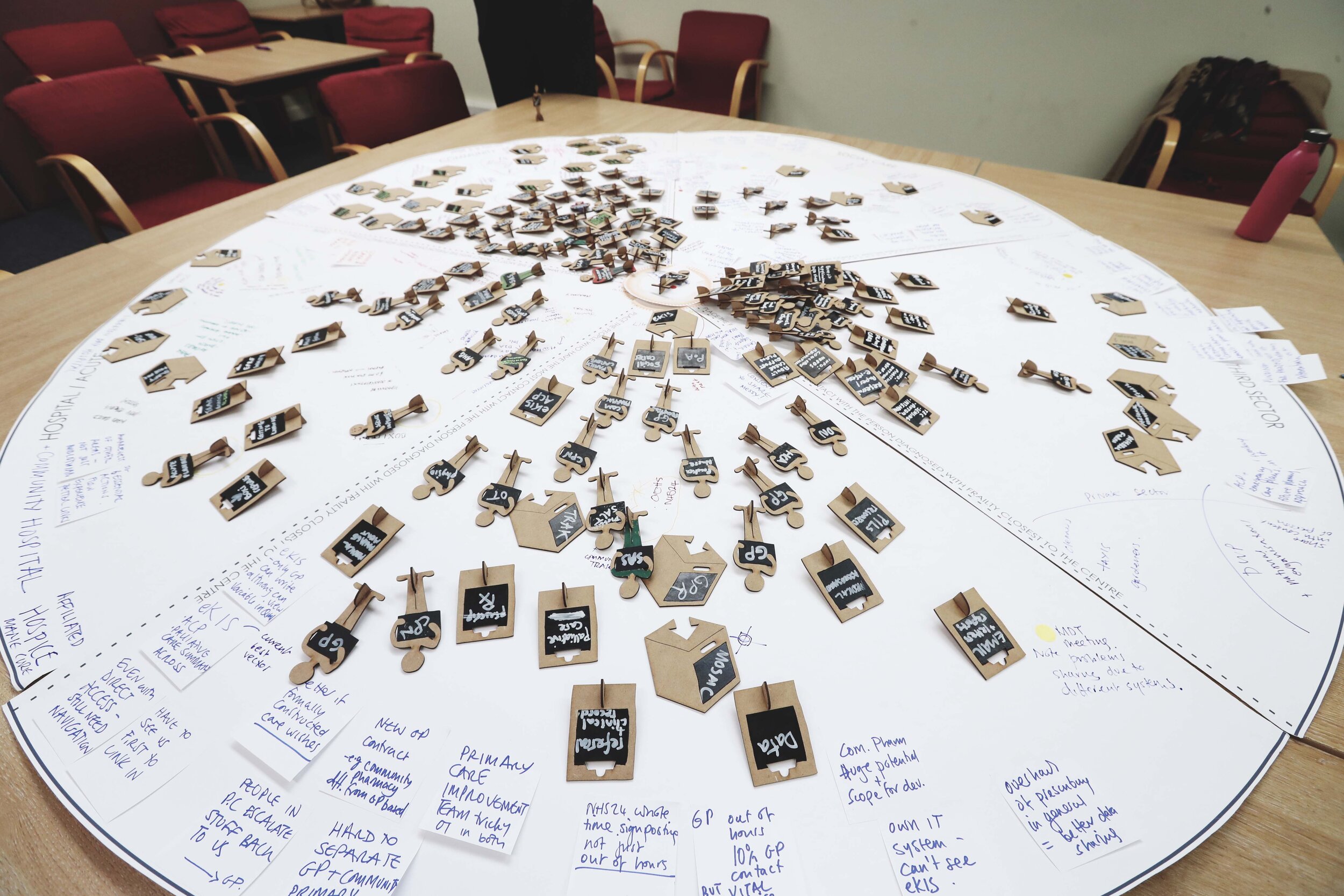
Images from a service mapping workshop in September 2019, all photography by Louise Mather
















In preparation for our engagements with people living with frailty and carers, we reviewed data gathered from previous local service evaluations and worked with colleagues to understand consultations that have already been undertaken around care for older people in Midlothian. Through this process, we identified the remaining questions that formed the basis of our in-depth interviews and public engagement with citizens. In parallel, we engaged widely with others working on frailty and identified key publications, best practices and individuals to light our path.
Before the pandemic, a system mapping workshop was held with multidisciplinary and multi-sectoral professionals delivering services for frailty in Midlothian. Researchers also observed a multidisciplinary frailty meeting and a British Red Cross ‘What Matters?’ frailty assessment in a person’s home to understand how these innovations support more integrated care and how these collaborative ways of working could be enhanced. We adapted the original engagement plan due to the COVID-19 pandemic, with planned pop-up engagement in public spaces redesigned to facilitate remote engagement using greeting cards and an online tool, and in-depth interviews with people living with frailty and carers taking place over the telephone.
KEY INSIGHTS
Through our discovery process, we learned that:
It is difficult to navigate the system to find the support you need for yourself or someone you care for.
Filling out forms and applying for services and benefits can be a barrier. Forms can be complex and intimidating and require you to share the same information many times.
Older people and carers value the people who help them navigate the system and apply for the things they need (in person or over the phone).
Keeping track of all the people and services and getting updates on progress can be challenging for older people and those who support them.
We defined eight questions that focused our design efforts through develop and deliver: ‘how might we support people…’
You can read in more detail about the findings of our discover and define phases here.
STAGE 2 - define & develop
In the next stage of the work, the project formed an ongoing working group with professionals from across Midlothian. The working group included health and care professionals, service managers, and third-sector professionals. A particular challenge that we faced in this phase of the work was understanding what could be done and what areas were best suited to technical innovation.
We carried out workshops with professionals over video conferencing, engaging their perspectives and thoughts on the experiences of people living with frailty and carers gathered from our in-depth interviews and undertaking service blueprinting sessions to give a detailed picture of how services currently provide support. These sessions discussed potential areas of opportunity, which we then explored with internal and external stakeholders to understand technical feasibility. Also in this stage, we undertook some focused interviews with carers to understand preferences around digital interactions and communications from services.
KEY INSIGHTS AND EMERGING CONCEPTS
Based on our further research, we found that many carers and older people preferred not to use digital services. This was for a variety of reasons, such as:
Lack of digital literacy and/or comfort with digital devices and interfaces
Accessibility issues common amongst older people, such as low vision
Digital fatigue from services going online during COVID
Feeling isolated and wanting to get out of the house and see others
Instead, we decided to focus on digital innovations that can support those who currently help people find the support they need to continue doing what they do best.
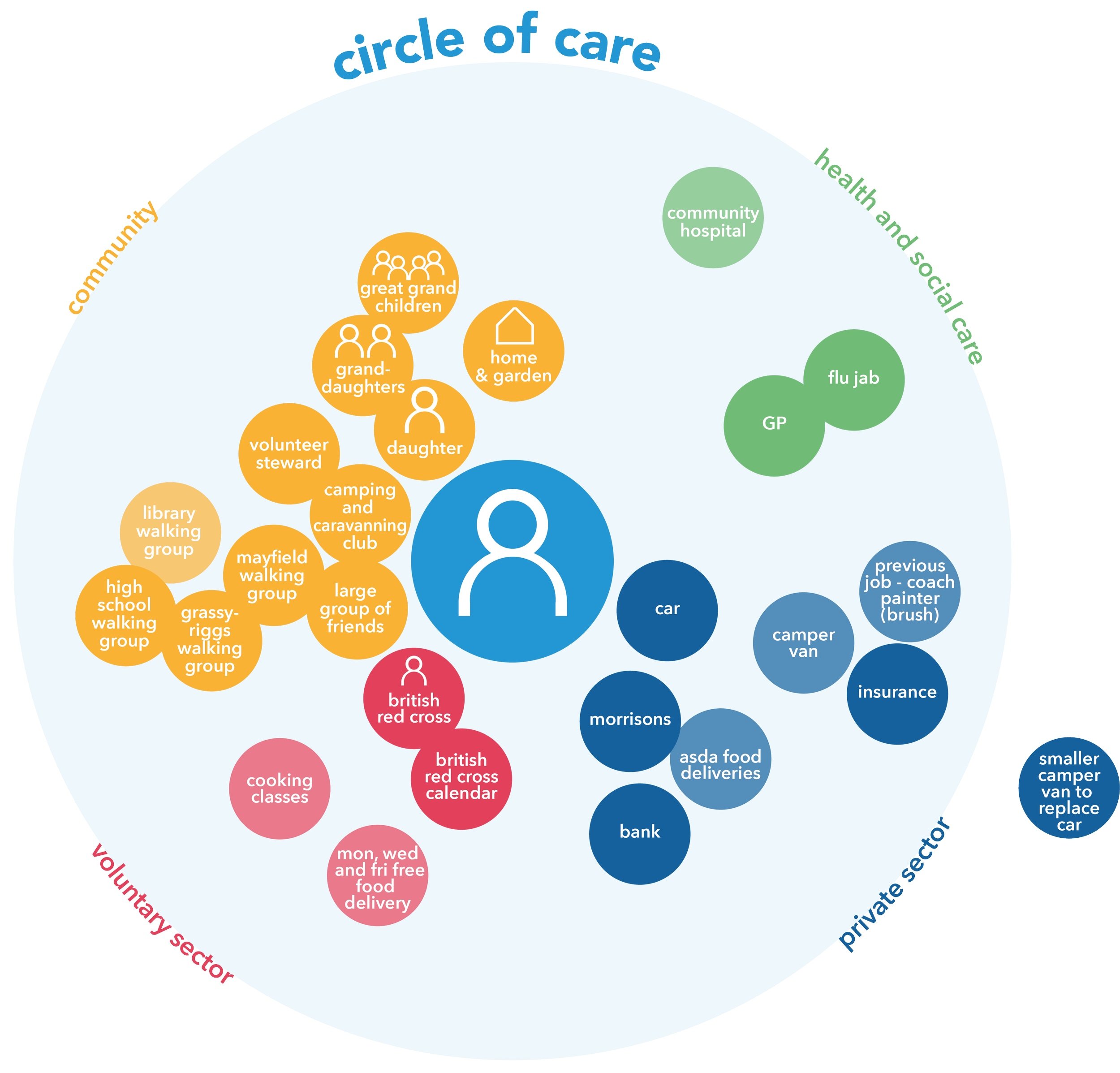
Building on our first stage of work, we identified an opportunity for our circle of care visualisations to play a role in supporting asset-based conversations, as they had in our interviews. Both citizens and professionals were enthusiastic about the visual representation as it helped them easily see and understand what support someone has in place. The circle of care became one of the project’s key concepts, visualising all the services and people supporting a person, with the individual themselves placed at the centre.
As a team, we saw the potential for this to become a digital tool for integrating care, sharing information and keeping track of appointments and referrals. Our frontline colleagues could see how this could be used as a tool within person-centred conversations, identifying possible gaps and new forms of support that could help. While we initially focused on how this could support professionals to help citizens navigate the system, we identified the potential for this to become an optional tool for carers and people living with frailty in the future.
STAGE 3 - develop & deliver
Through the insights gained from our engagement and co-design process, we built up a compelling and detailed ‘before’ story that described the current process and the challenges citizens and professionals face. This brought together different sectors of the frailty system, illustrating the information and communication flows (and barriers to this) across the system. To support this, we gathered all of the forms (e.g., assessment forms, referral paperwork) currently completed for the ‘before’ story and correlated this to identify all the data gathered about the person during this process. We layered onto our ‘before’ story all of the innovative concepts that emerged from co-design, our understanding of the ‘art of the possible’ drawn from DHI projects, and awareness of the future digital health landscape. This enabled us to create an ‘after’ story that was used to engage stakeholders and together agree the future vision for integrated care in Midlothian. Through collaborative prioritisation, we selected concepts to develop through iterative prototyping to help illustrate and develop a roadmap towards realising the future vision.
With the agreement of our working group, we selected the British Red Cross ‘What Matters?’ frailty assessment as a focus for our detailed development and prototyping. We worked closely with staff who undertake these assessments to understand how they expertly adapt the questions to create a person-centred conversation that gathers the information they need to support the person and make any onward referrals. We tried to build a representation of the logic behind the questions and the advisors’ expert knowledge of the system in identifying and actioning appropriate support in response to the person’s needs. This resulted in a prototype of a digital tool to support the assessment process, taking paper-based data collection and translating it into structured data that can be shared with other people and organisations with the person’s informed consent.
As part of this process, we returned to citizens and frontline staff at VOCAL and the British Red Cross to gather their feedback on the ‘after’ story and the concepts and prototype products and services created to help communicate what this might feel like.
KEY OUTPUTS
The underpinning technological innovation that enables the future vision was distilled into our Collaborative Care Architecture. We created a visual that explains how the different concepts come together to support person-centred information sharing, collaboration, access to services and integrated care. It removes the need for people living with frailty to retell their story to every new person they engage with. It largely automates form filling by reusing information and enabling digital ‘tokens’ to prove eligibility for services.
Collaborative Care Architecture enabling the vision for integrated care
We made several iterations of the Circle of Care prototype to learn about the functionality needed and how this could be used within conversations with professionals. There was interest among carers and people living with frailty to access the Circle of Care on their own devices and to use this to share information with family members living remotely. We explored options for ‘print and post’ functionality to enable the person to opt to receive a hard copy of the Circle of Care if they did not have access to online devices, both as a record of their conversation and to share with their family and friends.



We developed a prototype of the British Red Cross What Matters Assessment tool and showed how this linked to the Circle of Care to support person-centred and asset-based conversations. Key functionality for BRC and VOCAL advisors was the ability to automatically receive updates on the progress of referrals without making many phone calls. People living with frailty and carers were keen to access aspects of the assessment in advance of the What Matters assessment, for example, to see potential options for home adaptations and useful equipment. We documented our prototypes to support the development of specifications and future development.
Finally, our data mapping activity resulted in a ‘data dictionary’ containing every data item captured in every conversation, form or tool in a single spreadsheet. This creates a ‘master’ data model for frailty, which is key to enabling integration and data sharing across different services and sectors.
SHARING INSIGHTS ACROSS THE DHI PORTFOLIO
The lived experience insights, collaborative care architecture, key concepts and data model created as part of this project have been explored and validated in Moray as part of the DHI Rural Centre of Excellence for digital health and care innovation funded by the Moray Growth Deal. This has led to the development of tools to support carers in Moray, which will be implemented as part of a test of change in early 2024.
NEXT STEPS
We are working to build momentum and realise the future vision through national engagement and collaboration. This will involve a period of validation with other regions to understand if what we have found and developed in Midlothian and Moray has wider applicability. Early conversations show excitement and appetite for this kind of transformational change to better meet the needs and aspirations of citizens.
Further Information
For more information about this project please contact:
Matthew Curl, Matthew.curl@nhslothian.scot.nhs.uk
Gemma Teal, G.Teal@gsa.ac.uk
Marissa Cummings, M.Cummings@gsa.ac.uk
Cate Green, C.Green@gsa.ac.uk