PERSON-CENTRED RECORDS: quarter 1
Exploring the potential of in-patient electronic working in NHS Grampian
In the 1st quarter of our research project activity, several interviews, focus groups and a co-design workshop have been undertaken to gather understanding of NHS Grampian's current record keeping practices and processes and start generating co-produced ideas for a future electronic record keeping system for person-centred in-patient care. ‘Person-centred’ means focusing on the staff delivering and patients using the NHS Grampian in-patient services. This is as opposed to focusing on technology or auditing requirements.
Below are six themes identified from early focus groups and interviews with allied health professionals (AHPs), medical staff and nursing staff (from junior to director levels). These themes were used at the first co-design workshop as a focal point for group discussion. Emerging ideas and issues are then described through a collection of illustrated concepts. The ideas and concepts shown here are for speculation and provocation and will inform the subsequent co-design workshops. Several ideas presented here are addressed by the NASSS framework which is a series of questions useful for evaluating the non-adoption or abandonment of new technologies and digital services in health and social care settings. It is presented here as a pre-assessment tool for considering the future success of possible changes in record keeping practices and a future innovative record keeping system. The pertinent NASSS framework questions are shown in full and should be considered at this early stage.
The concepts shown below are separated into two categories: changing the way in which staff work and possible properties of a new record keeping system. Finally, a number of suggested design principles are shown which represent the approach to implementing new processes and systems. The following report and its content has been produced by the design research team who are external to NHS Grampian. This is a report on the first quarter of research activity of the Person-centred Records project. A summary of this report can be downloaded here. There is also a report on the 2nd quarter of project activity.
Themes
From initial focus groups and interviews with nursing staff, AHPs and medical staff, six themes have emerged and were used to frame co-design workshop one. These six themes are illustrated below:
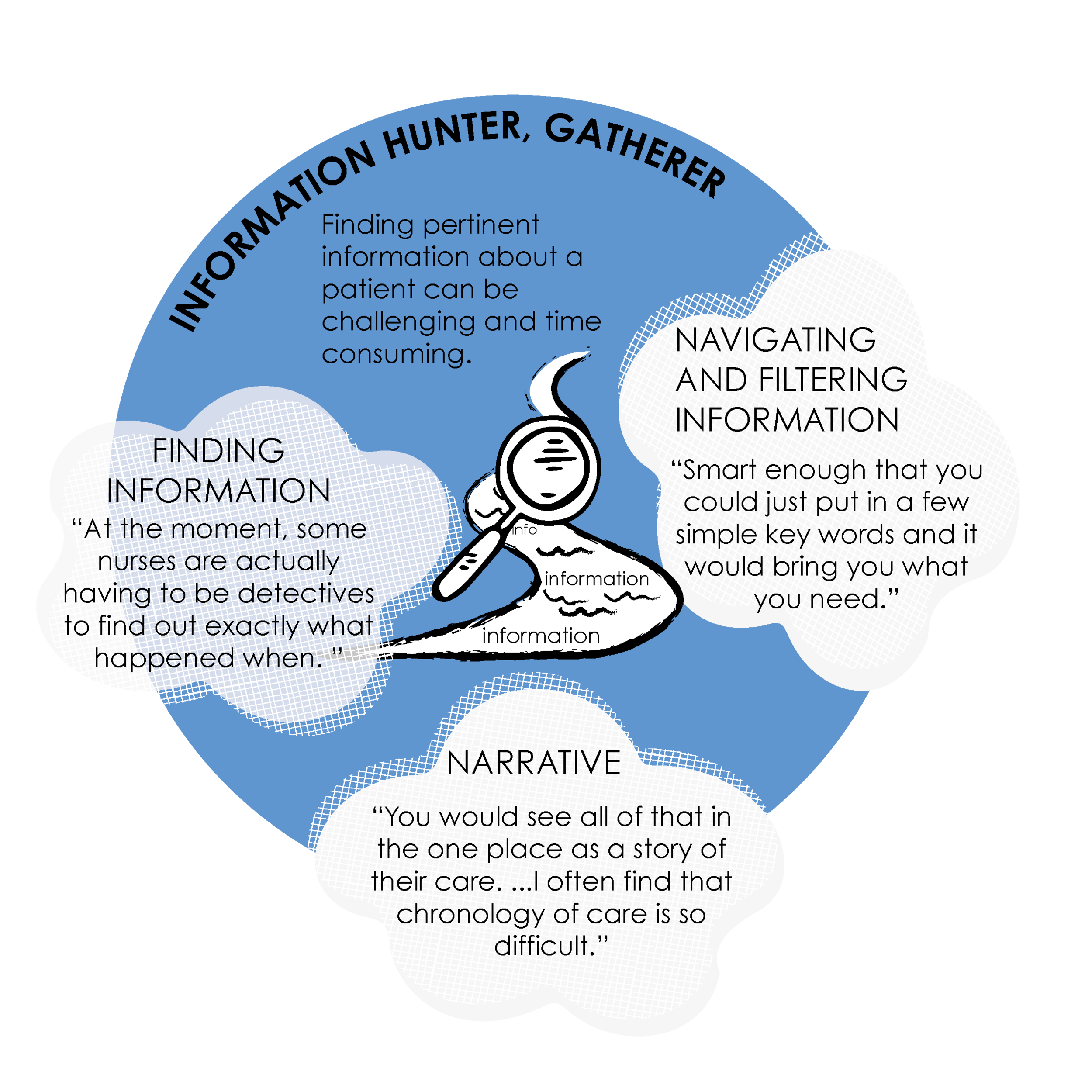
1. INFORMATION HUNTER-GATHERER
Finding pertinent information about a patient can be challenging and time consuming.
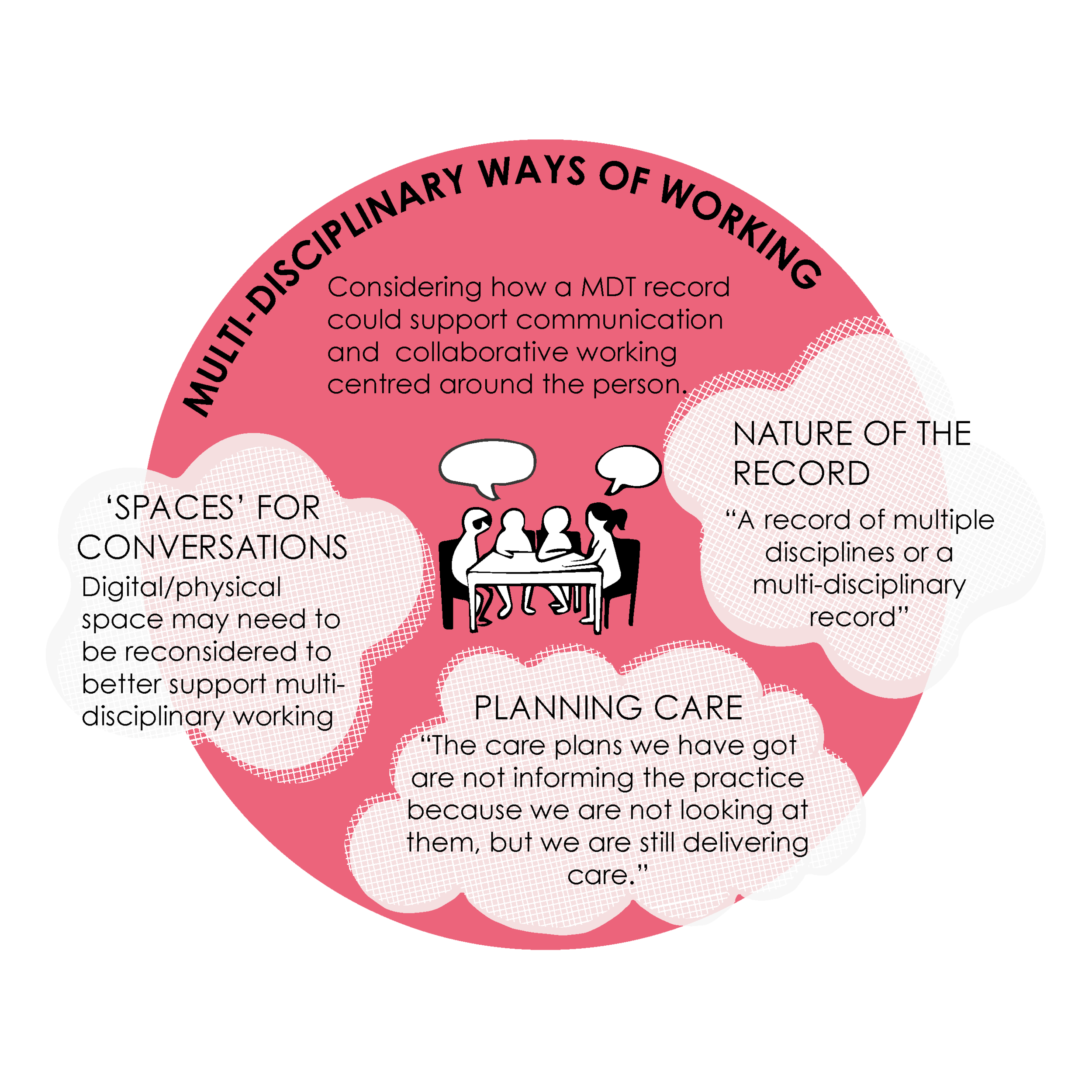
2. MULTI-DISCIPLINARY WAYS OF WORKING
Considering how a MDT record could support communication and collaborative working centred around the person.
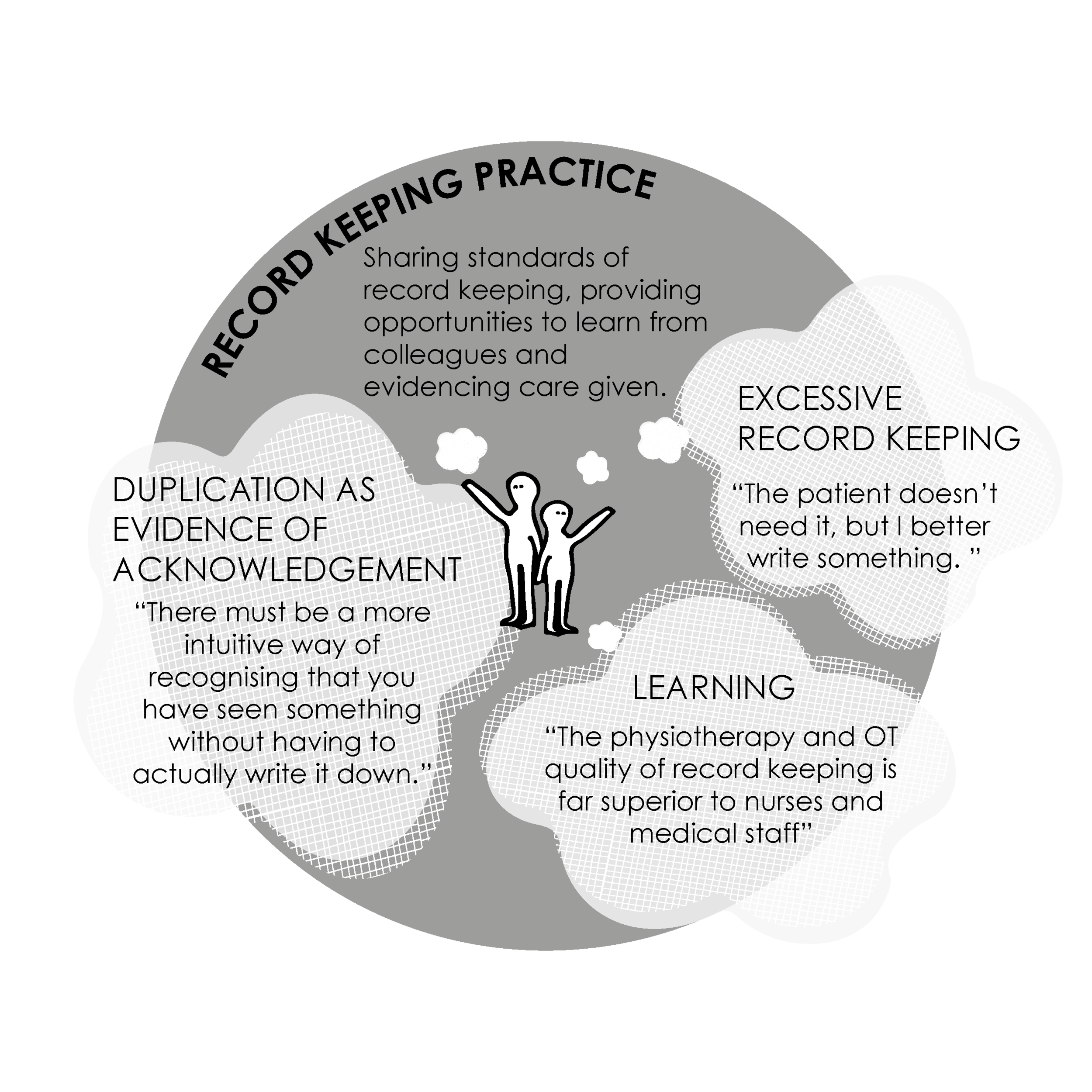
3. RECORD KEEPING PRACTICE
Sharing standards of record keeping, providing opportunities to learn from colleagues and evidencing care given.
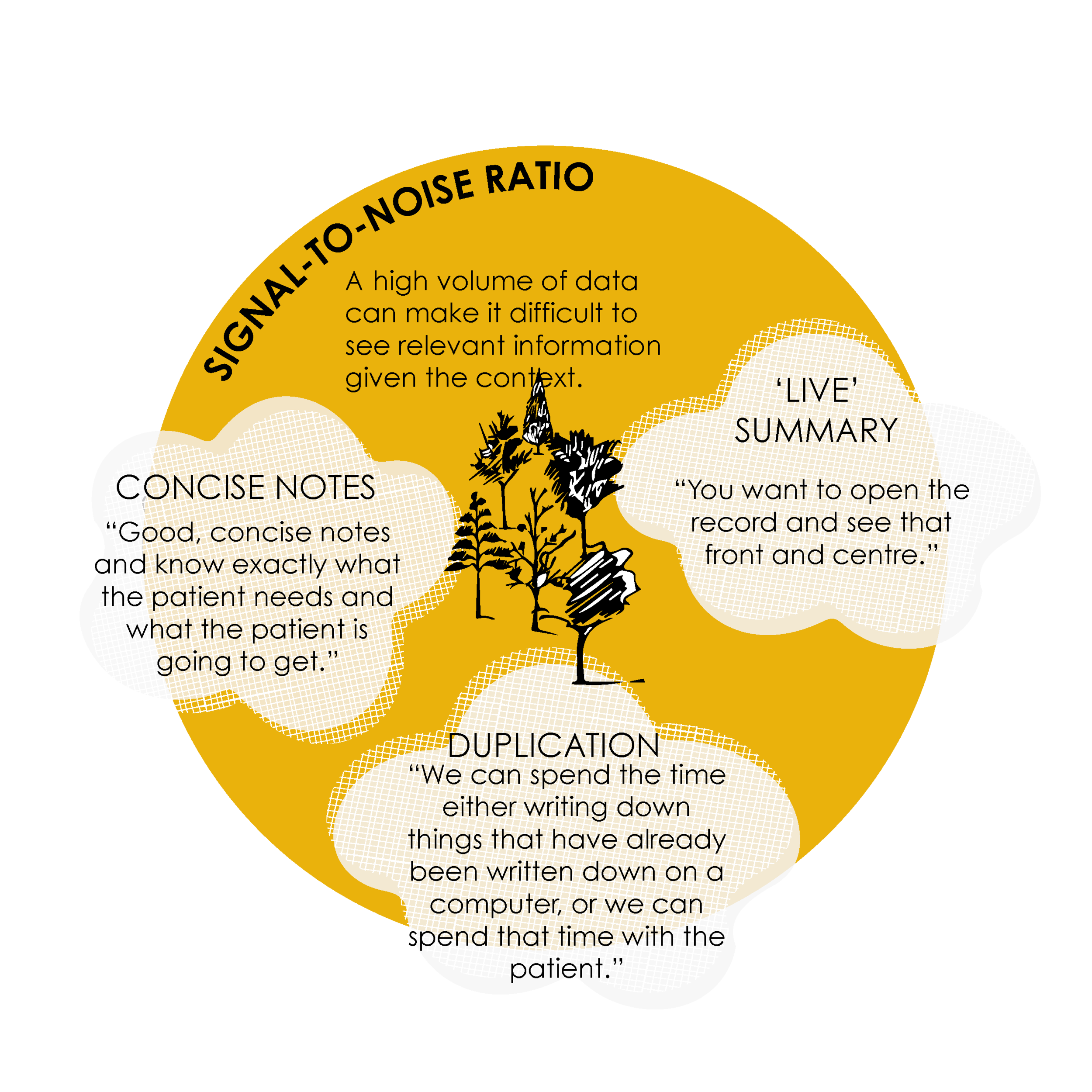
4. SIGNAL-TO-NOISE RATIO
A high volume of data can make it difficult to see relevant information given the context.
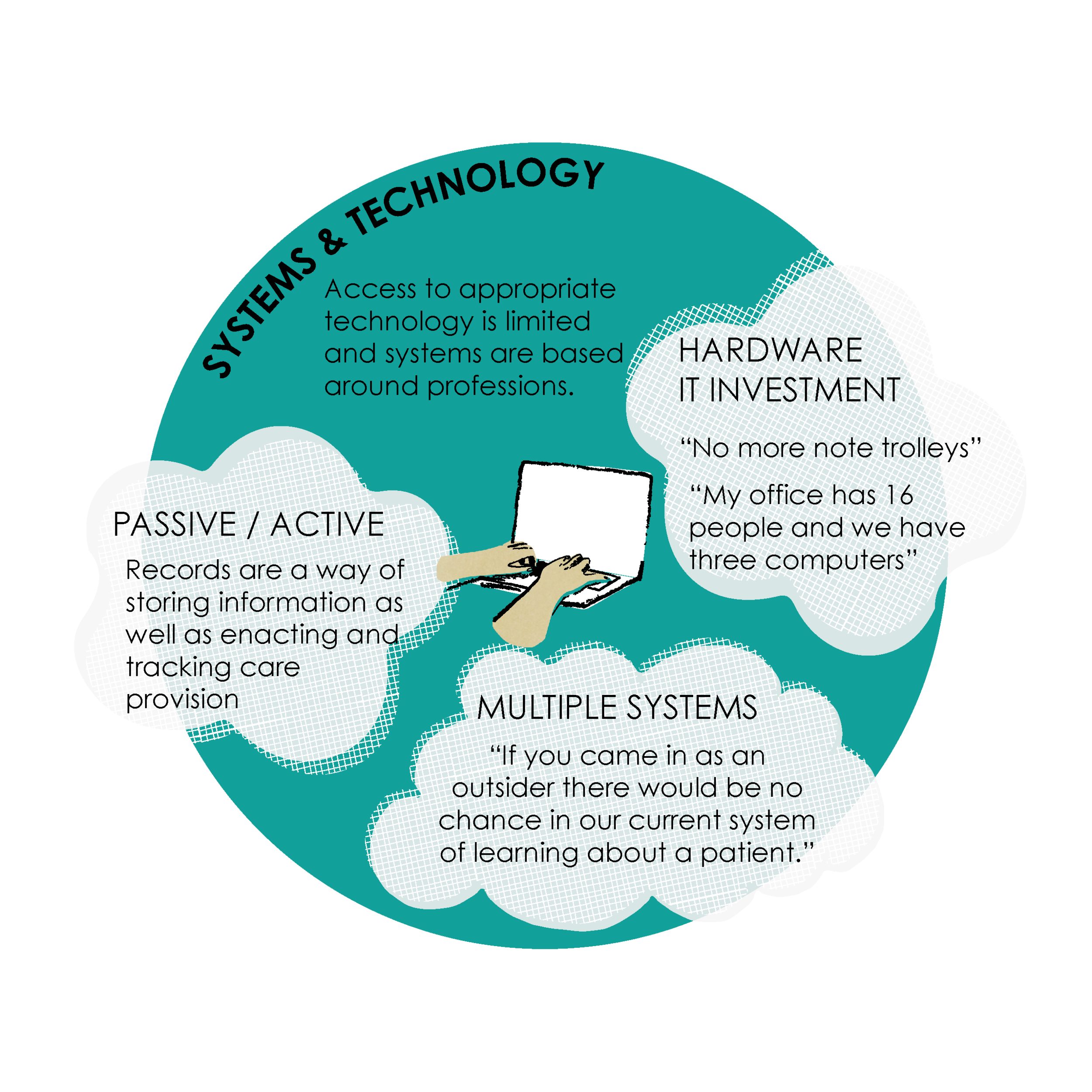
5. SYSTEMS AND TECHNOLOGY
Access to appropriate technology is limited and systems are based around professions.
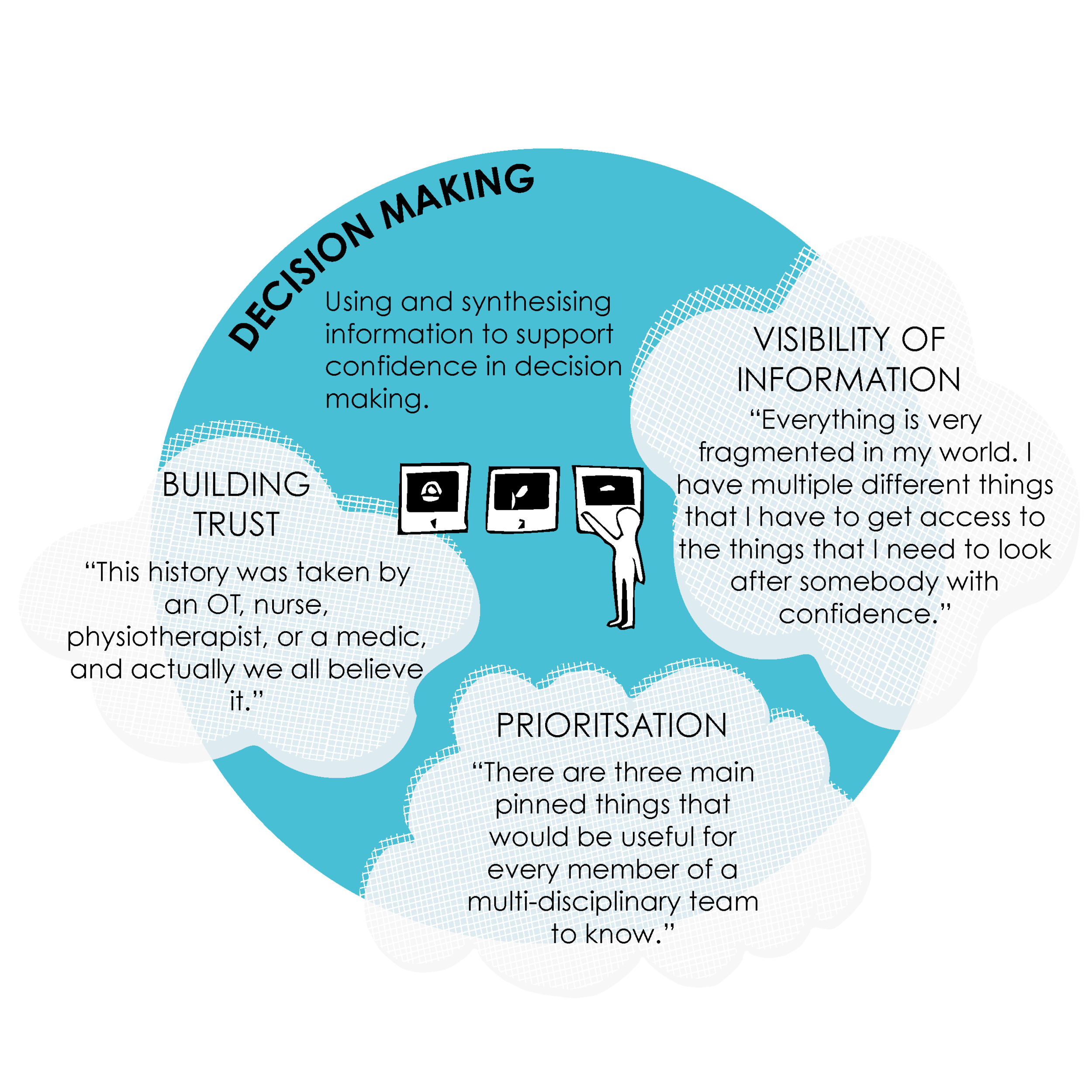
6. DECISION MAKING
Using and synthesising information to support confidence in decision making.
CONCEPTS
The following concepts are split into two categories: ways of working and system requirements. These concepts have come from participants at interview, within focus groups and at the first co-design workshop. These concepts are intended as speculative designs and will inform further discussion at future workshops within this research project.
Ways of Working
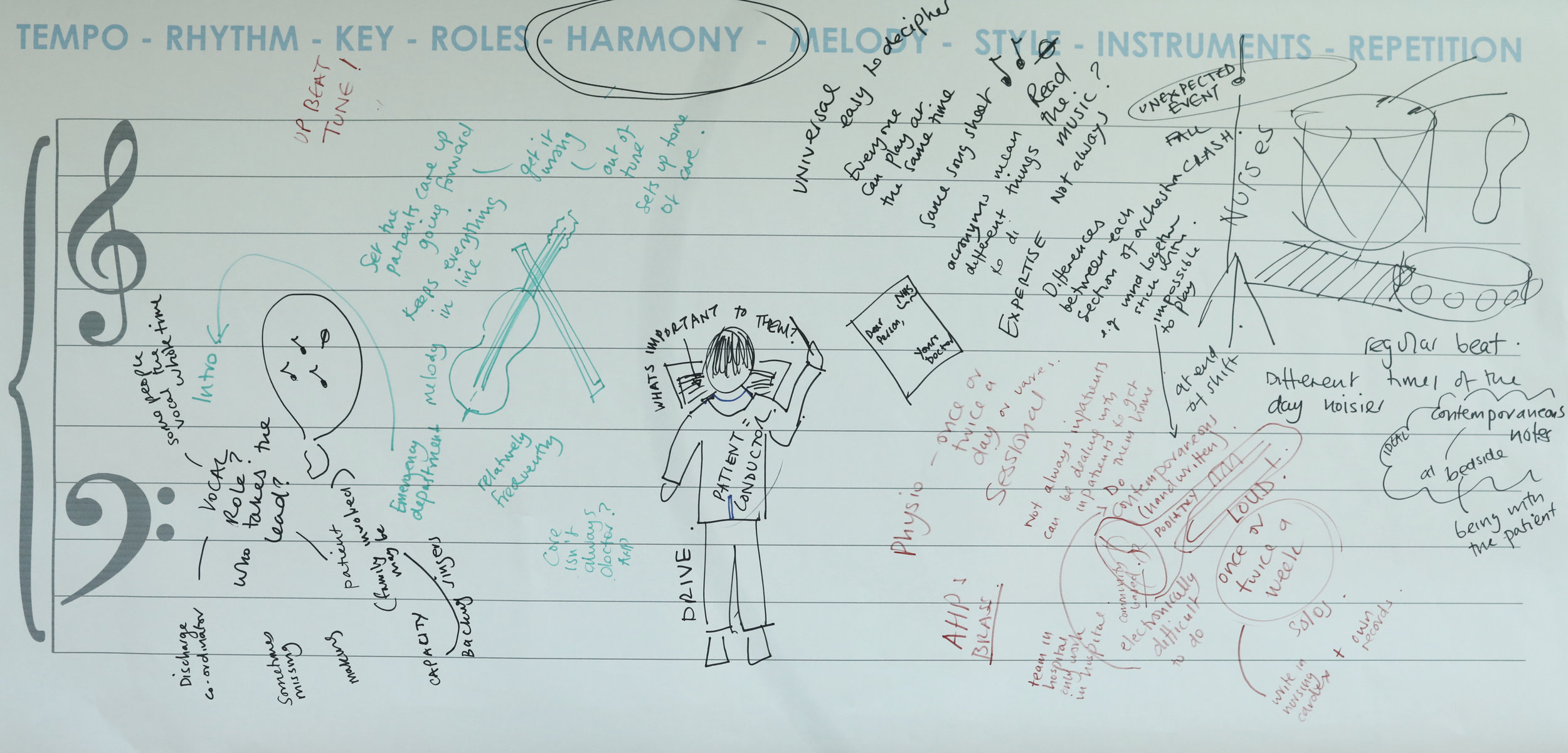
Multi-disciplinary record keeping may be new to many staff at NHS Grampian but even if staff are familiar, there is still an opportunity to design a preferred way of multi-professional working with electronic records. Participants at the focus groups and workshop showed a desire to involve the patient in the planning of their care in some form. The level of involvement (or ability) of the patient could be assessed at admission. Whether patients arrive via the emergency department or come for planned care may affect their ability or willingness to be a more active participant in their care while an in-patient. Participants asked if patients could be educated to be more active and suggested that.
“What you write in the record is what you say to the patient.”
The goals of a multi-disciplinary in-patient team was seen to be significant. Participants discussed the needs of the patient as the focus for determining a joint plan of care and highlighted that the value perceived by the staff and the patients is what should drive the record keeping process (as opposed to auditing for example).
Participants also raised the issue of multiple consent and whether each specialism needed to take consent which could be seen by the patient as unessesary duplication. Would it be possible for the patient to consent to in-patient care? Finally, the use of language was seen by participants as potentially problematic with the need to avoid conflicting abbreviations and use plain language to communicate across the multi-disciplinary team. The patient could be used as a proxy for standards of language.
“What is important to the patient is important to us.”
Supporting continuous decision making
An in-patient’s journey can be viewed as a continuous series of decisions. Through making visible the evidence leading to a decision point and resultant actions, we can more easily track and share patient care with colleagues.
Phases of inpatient care
In-patient staff work on three general activities which the records keeping system should specifically support: admission, continuous care and discharge. These activities are non-linear and distinct. For example, admission may be spread over several professions at different times and discharge planning should start during admission. Each phase has information particular to it (e.g. admission document, handover sheets or core discharge document). The future system should be built to promote the flow of information into each task (e.g. discharge).
“Particularly in in-patient environments we have multiple disciplines working in the same environment, separately, and they all have their own priorities, they all have their own tasks, but in many situations fail to coalesce around really whose agenda is the most important: which is the patient’s.”
Conversation tool
In discussing a desired way of working, participants highlighted a desire for a record keeping system which enables communication through supporting the therapeutic relationship and enhance inter-professional relationships. A notification and flagging system could remove much of the perfunctory communication (e.g. ‘phone tennis’ and waiting around to catch colleagues as they come and go) and leave more room for discursive communication or team activities (e.g. decision making).
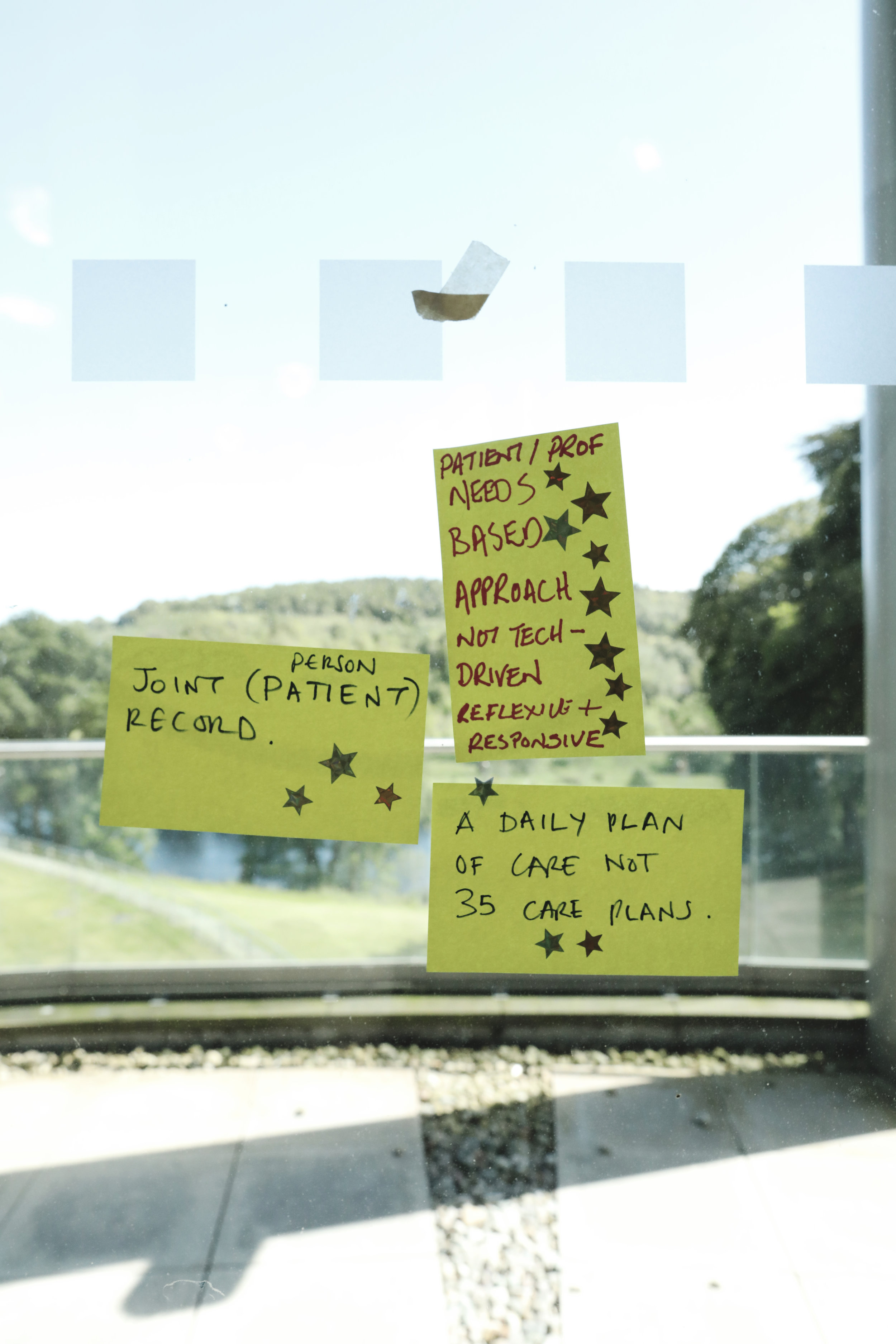
Planning Care
Multiple care plans could be replaced by a joint plan of care used by all specialisms throughout the in-patient's journey. Updates would be made jointly.
VALUE
Auditing should not be the primary driver for record keeping activities, instead we should focus on the value for the patients and professionals. Through having a visible record of the patient journey, the decisions and actions, auditing can take place in the background rather than explicitly undertaking activities for the purposes of audit.
What is assessed to be valuable for the patient and health professional should satisfy audit requirements. An assessment of record keeping activities could be carried out for the yet-to-be-designed system to decide how much value each activity contributes to in-patient care and the in-patient team.
“The level of duplication is collosal.”
System Requirements
There are two distinct modes to record keeping systems: passive and active. The records are a passive store of information and there may be functionality such as searching and different views such as timelines and summaries of this data. There are also active parts of the record keeping system such as requesting procedures, tests and other staff to carry out actions. It might be useful to keep in mind which of these modes we are considering when making changes.
A number of views have been suggested by workshop participants as being potentially useful: timelines of care; thematic (i.e. specialisms); a view specifically to support shared decision making (including information gathering and assigning actions); a 'front page' common to all staff/patients; and one or more summary views as yet to be determined.
Key to design and implementation will be the controlling logic which joins the views to the model (i.e. the interfaces to the data). The possibilities of using the TrakCare API is yet to be investigated.
TrakCare will continue to be used by NHS Grampian and so it is assumed will continue to act as a data-store. Many digital systems are developed according to the model-view-controller architecture in order to allow slippage between components during new developments. Many of the concepts are still to be developed at this stage and whether they are built using TrakCare or as a new collection of interfaces is still to be determined. It appears that TrakCare does have significant functionality and is extensible and so it may be that the new interfaces could be made using the existing or an extended version of TrakCare.
Notifications and action flagging
Instructional communication can be replaced by a flagging and notification system. Actions to do can be assigned to members of staff, teams or roles. Individuals can decide what is suitable for flagging to other staff. That is, what other staff should be aware of about a patient.
“What do I need to know?”
Multiple systems
The use of multiple systems makes it difficult for staff to do their job, to the detriment of patient care. Participants discussed a need to reduce the number of systems that in-patient staff must access to perform their roles. Should we be putting effort into improving or remodelling existing systems (i.e. TrakCare) to match our expectations or should we be introducing another system? If a new system were to be introduced then it could only be justifiable if it reduces the number of systems staff must interact with. That is, it should amalgamate other existing systems from the point of view of the staff. The NASSS framework, question 2D , addresses this aspect of implementation: is TrakCare extensible enough to add new features (yet to be identified) or would a new system need to be built.
“Make it easy to do the right thing well.”
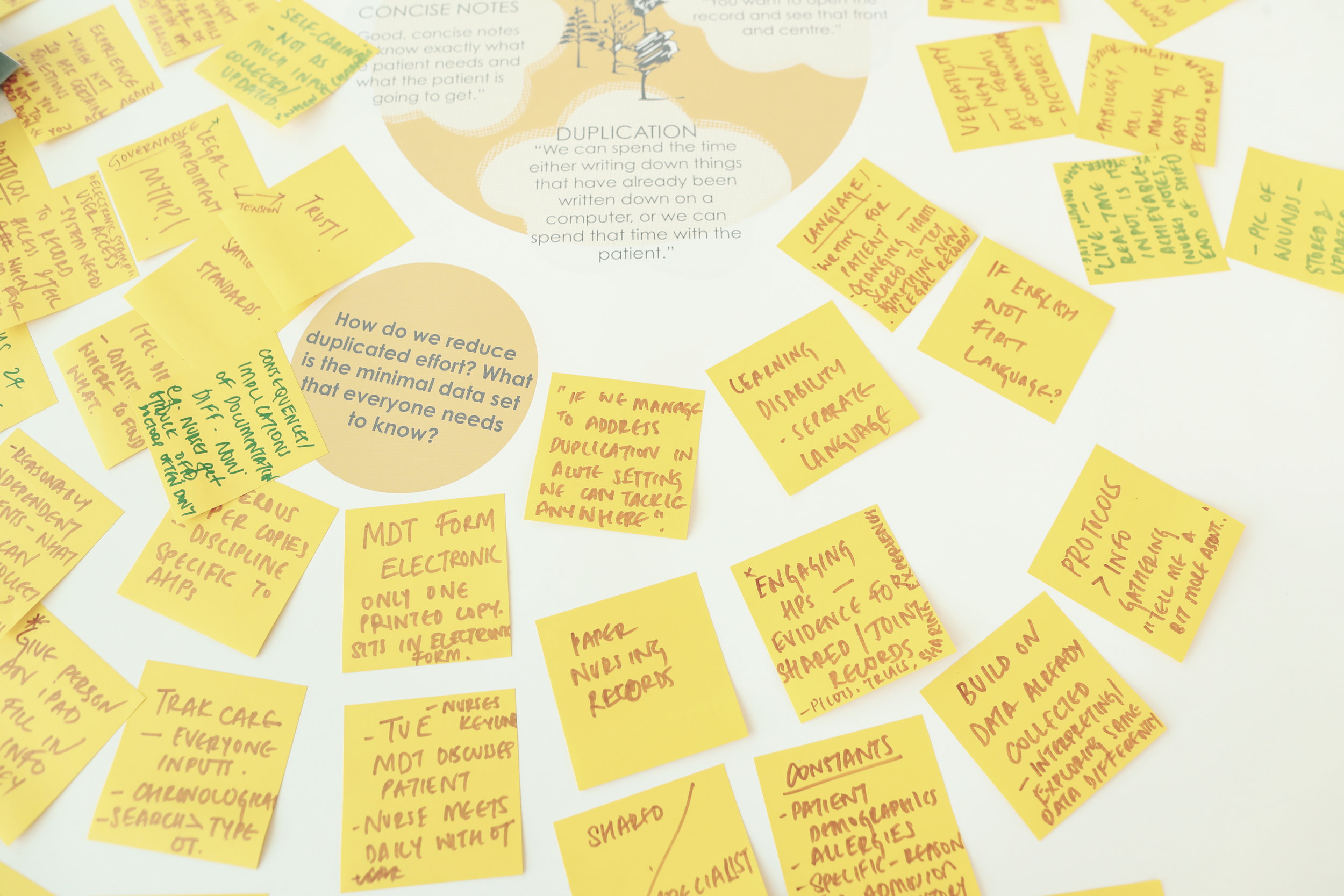
Photographs from the 1st workshop in Aberdeen on the 18th June by Louise Mather at no middle name.
The Nature of the Record
Basic v's advanced properties
There is a clearly defined goal to move to electronic records within NHS Grampian. There are some aspects of record keeping that are improved purely by moving to electronic record keeping. These could be described as coming 'for free' and are basic expectations of modern electronic record systems (but still rely on the appropriate implementation). This aligns with a question 2A from the NASSS framework. In our case the co-location of all records should be one of these basic properties. Issues finding information would be improved simply by having the records of all professions (or a sufficient sub-set of each profession's records) in one single, accessible place. An interface showing a tab for each of the approximately 72 professions involved in in-patient care would be a significant improvement over the predominant use of paper records. However, this interface would highlight the significant non-systems challenge of this research: changing the way in which multi-disciplinary teams work together.
“A record of multiple disciplines or a multi-disciplinary record?”
What are the key features of the technology?
NASSS Framework Question 2a
Simple: Off-the-shelf or already installed, free-standing, dependable
Complicated: Not yet developed or fully interoperable; not 100% dependable
Complex: Requires close embedding in complex technical systems; significant dependability issues
Basic expected properties
We would expect any future electronic system to provide: a massive reduction in duplication; a standard process and interface for entering and retrieving information; reducing loss of information in the records (compared to paper notes) and; searching and/or filtering functionality. There is an opportunity within the future system to use colour coding to highlight different professions as was seen in the past with colour-coded sections for different specialities.
Complex Properties
There are many more complicated issues around the way in which in-patient staff work effectively as a multi-professional team (and this includes the possible inclusion of the patient in that team). The most significant change that a future record keeping system would support is that of multi-disciplinary team working. ( NASSS framework 4a ) It may be sufficient to move to an electronic record keeping system that will improve certain aspects of in-patient working practice without actually changing the way in which staff work. However there is an obvious desire and there appears to be many benefits of moving towards a more multi-professional way of working. Other significant advanced topics that could be addressed by a future electronic record system would be: the change in culture to more open, shareable records; the programmatic use of the data for functions such as audit and 'auto-magically' produced view content (such as summaries and timelines).
What changes in staff roles, practices, and identities are implied?
NASSS Framework Question 4a
Simple: None
Complicated: Existing staff must learn new skills and/or new staff be appointed
Complex: Threat to professional identity, values, or scope of practice; risk of job loss
Guiding Design Principles
The workshop activities colminated in co-designing a set of design principles that the single, multi-disciplinary, electronic record for inpatient care should work towards. These are intended to guide the development of the future innovation and are subject to change as the understanding of requirements becomes more refined.
INNOVATIVE RATHER THAN AN E VERSION OF NOW
TOOL TO SUPPORT DECISION MAKING AND PLANNING CARE
WORKING TOGETHER TOWARDS A COMMON GOAL
NOT DUPLICATING BUT BUILDING ON AND SHARING INFORMATION
FOCUS ON PATIENT / PROFESSIONAL NEED RATHER THAN TECHNOLOGY
INNOVATION ADOPTION BARRIERS
There are two significant potential barriers to introducing innovative record keeping practices and systems within the in-patient department at NHS Grampian: funding and institutional readiness.
Funding
There will be a funding gap when moving to electronic record keeping systems. Aside from indirect costs such as training there is a significant lack of access to electronic devices to enter and retrieve records. This is a major blocking problem and is identified in NASSS framework questions 5C and 5E . Can a funding decision be made and who will implement the changes? A funding model will need to be identified and the value proposition is central to this. Questions 3a and 3b from the NASSS Framework considers these points.
What is the developer’s business case for the technology (supply-side value)?
NASSS Framework Question 3a
Simple: Clear business case with strong chance of return on investment
Complicated: Business case underdeveloped; potential risk to investors
Complex: Business case implausible; significant risk to investors
What is its desirability, efficacy, safety, and cost effectiveness (demand-side value)?
NASSS Framework Question 3b
Simple: Technology is desirable for patients, effective, safe, and cost effective
Complicated: Technology’s desirability, efficacy, safety, or cost effectiveness is unknown or contested
Complex: Significant possibility that technology is undesirable, unsafe, ineffective, or unaffordable
Institutional readiness for innovation
Domain 5 of the NASSS framework (5c and 5e) considers the organisation itself (NHS Grampian) and its ability to support innovation. The NASSS framework conflates lack of leadership with lack of 'slack resource' and this is not the case for this project. NHS Grampian may not have what the NASSS framework calls 'slack resource' (spare computers, extra budget, staff with unallocated time, etc.) but it is a 'well-led organisation' and the directors support the in-patient electronic working efforts.
How easy will the adoption and funding decision be?
NASSS Framework Question 5c
Simple: Single organisation with sufficient resources; anticipated cost savings; no new infrastructure or recurrent costs required
Complicated: Multiple organisations with partnership relationship; cost-benefit balance favourable or neutral; new infrastructure (e.g., staff roles, training, kit) can mostly be found from repurposing
Complex: Multiple organisations with no formal links and/or conflicting agendas; funding depends on cost savings across system; costs and benefits unclear; new infrastructure conflicts with existing; significant budget implications
What work is involved in implementation and who will do it?
NASSS Framework Question 5e
Simple: Established shared vision; few simple tasks, uncontested and easily monitored
Complicated: Some work needed to build shared vision, engage staff, enact new practices, and monitor impact
Complex: Significant work needed to build shared vision, engage staff, enact new practices, and monitor impact
“It’s imperative that we create a multi-disciplinary set of guidance around record keeping.”
Governance landscape
Institutional readiness extends to the professional bodies for nursing, medical and AHP staff. No single governing body is responsible for setting multi-disciplinary working standards and protocols. A cross-disciplinary body within NHS Grampian may need to take on the role of setting best practice for MDT record keeping.
POP-UPS at Excellence in Care Events
In order to more widely share our progress and gather further insight we have scheduled a number of pop-up interventions throughout the project timeline at the Celebrating Excellence events going on across NHS Grampian. These events have allowed us the opportunity to pose questions and provocations around how a multi-disciplinary, electronic record keeping system might better support people in their professional roles, multidisciplinary record keeping guidelines and decision making. The responses and resulting conversations can then be knitted back in to the co-design workshops.
Celebrating Excellence Events
Currently there is no single governing body responsible for setting multidisciplinary working standards and protocols. How might the future governance landscape support multi-disciplinary record keeping?
An inpatient’s journey can be viewed as a continuous series of decisions. It is important to make visible all the evidence leading to a decision point and the resultant actions. How might this enhance inter-professional relationships and support a therapeutic relationship with patient?
Project Activity
NEXT STEPS
A further three design-led workshops are planned for the 2nd quarter looking at some of the concepts and ideas shown above. These workshops will give a better understanding of how NHS Grampian staff would prefer to practice multi-disciplinary record keeping within in-patients.
A further three workshops in the third quarter of the project will look specifically at the simulation of a preferred new electronic records system with staff. These workshops will validate or challenge earlier decisions and produce requirements for a new or extended electronic record keeping system.
The research team are planning to run a series of observation sessions within NHS Grampian hospitals to visually document typical staff interactions with records.
Finally (April 2020), we will produce recommendations for preferred ways of MDT working supported by electronic records and the requirements for a new or extended electronic record keeping system.
Authored by Jay Bradley and Angela Bruce from the Digital Health & Care Institute/ Innovation School at the Glasgow School of Art, July 2019.