PERSON-CENTRED RECORDS: quarter 2 Report
Preferred Ways Of Multi-Disciplinary Record Keeping
This report covers the ongoing activity of co-design workshops run in the second quarter of the year-long Person-centred Records project. Please note that this report has been produced by researchers in partnership with NHS Grampian staff and the following content serves only as recommendations made to NHS Grampian.
A series of three design-led workshops were undertaken with NHS Grampian staff to co-design a future electronic record keeping system for person-centred, in-patient care. Through the use of bespoke tools, staff were asked to collaboratively evaluate the current systems and information collected in terms of its value to patient care and in-patient staff; to discuss their aspirational ways of working together; and consider the role an innovative digital record could play in supporting this. Each workshop built on the insights from the previous design activities to develop ideas and understanding further, towards a future vision of a MDT record and a basic prototype. The second quarter activity timeline is shown at the end of the report. Future research activity in the third and fourth quarters will include prototyping and validation of the work so far. A summary of this report is available here.
Preferred Ways of Multi-disciplinary team working
Based on the findings in the first quarter report and a high-level review of similar use cases, the NHS Grampian staff participants were asked to consider how we might move away from “managing documents” towards “managing relationships” [Ramsay and Seth, 2017]. Firstly, staff were asked to consider their current record keeping systems and the information that informs how they work and then reflect on the value of this information. Secondly, participants were asked to think about the multi-disciplinary planning of care around a person and their goals while an in-patient.
Value of data
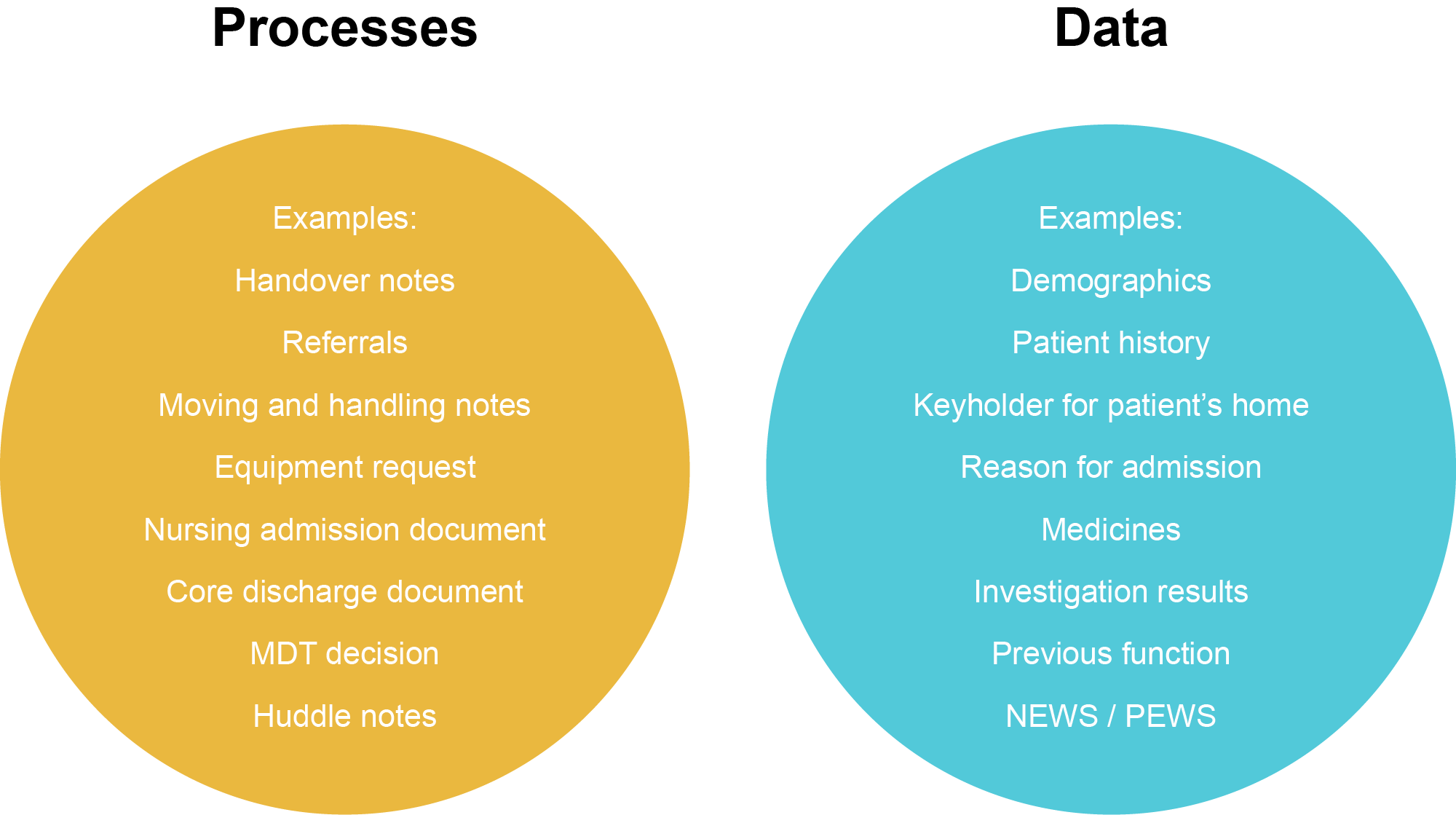
Participants were asked to consider and discuss what data they gather during a typical in-patient stay and record examples on cards provided (as shown below).
Data or process
Participants suggested many processes instead of data. i.e. processes such as nursing admission instead of bits of information relevant to the patient such as investigation results. This suggests a thought process that is focused on process rather than data. Processes will produce data but they are not data themselves. In future work to re-design record keeping staff should rethink record keeping to be centred around a shared set of data relevant to the patient which is decoupled from their healthcare processes specific to in-patient care. For example, AHP and nursing admissions are different processes but the same data may be collected during each process. It may be that the focus on process reinforces a perceived difference between data collected by staff from different specialisms.
Many systems
Participants contributed data stored on a variety of paper, TrakCare and other electronic systems.
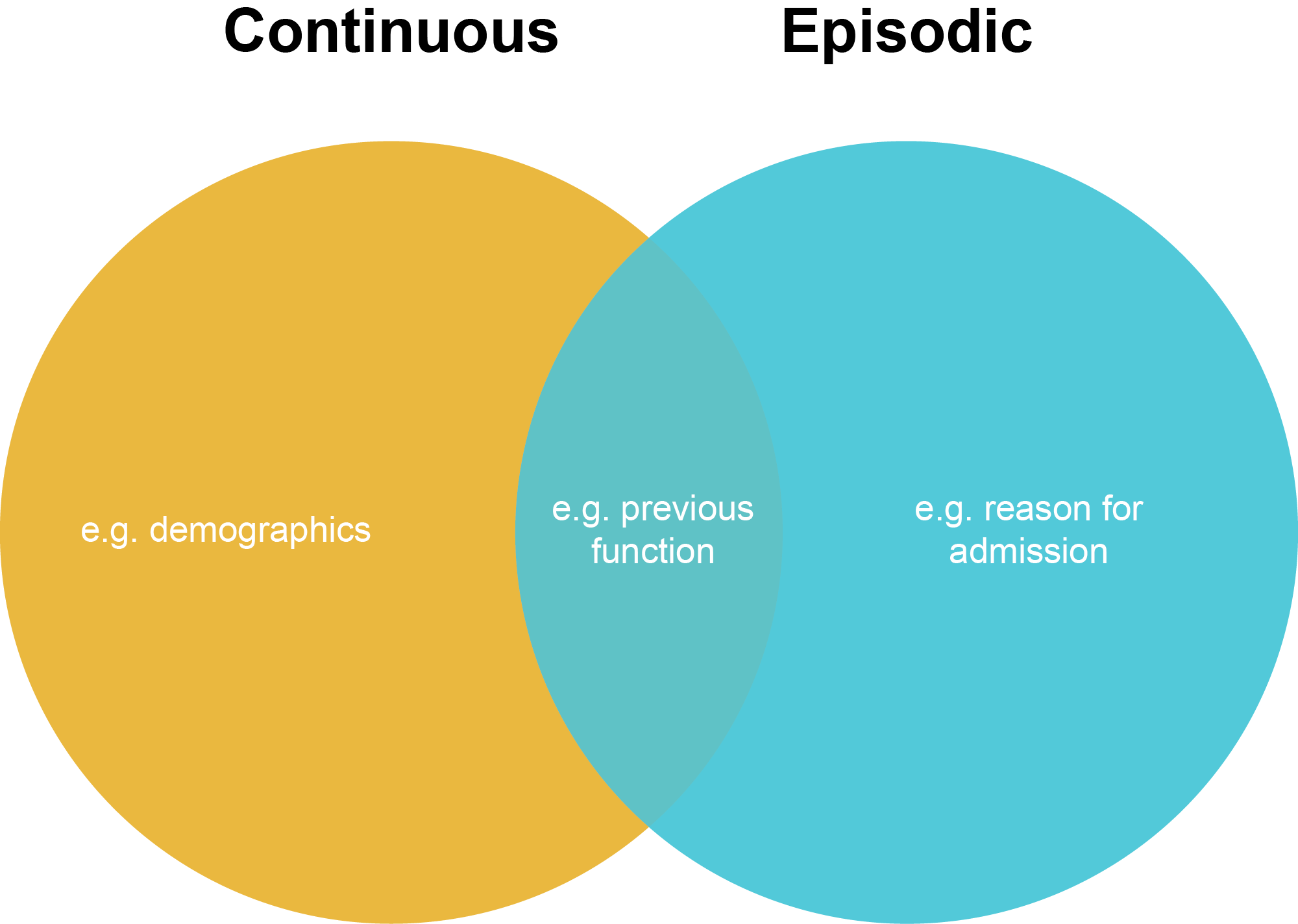
Continuous or episodic
Participants suggested patient data that could be categorised as relatively permanent such as demographics or as relatively transient such as investigation results. In-patient visits are by their nature episodic but some data outlasts an in-patient stay. It may be helpful to think of patient data as belonging to a continuous record of care or an episode of care. These sets of data could be presented to staff differently to reinforce the distinction.
Documenting, communicating and caring and treatment
The purposes for recording data as suggested by the participants fell into three categories: documenting (for historical, proof or audit reasons); communicating (to staff or patients) and; caring for and treating the in-patient for the condition(s) for which they were admitted.
Planning Care: Aspirational Ways of Working
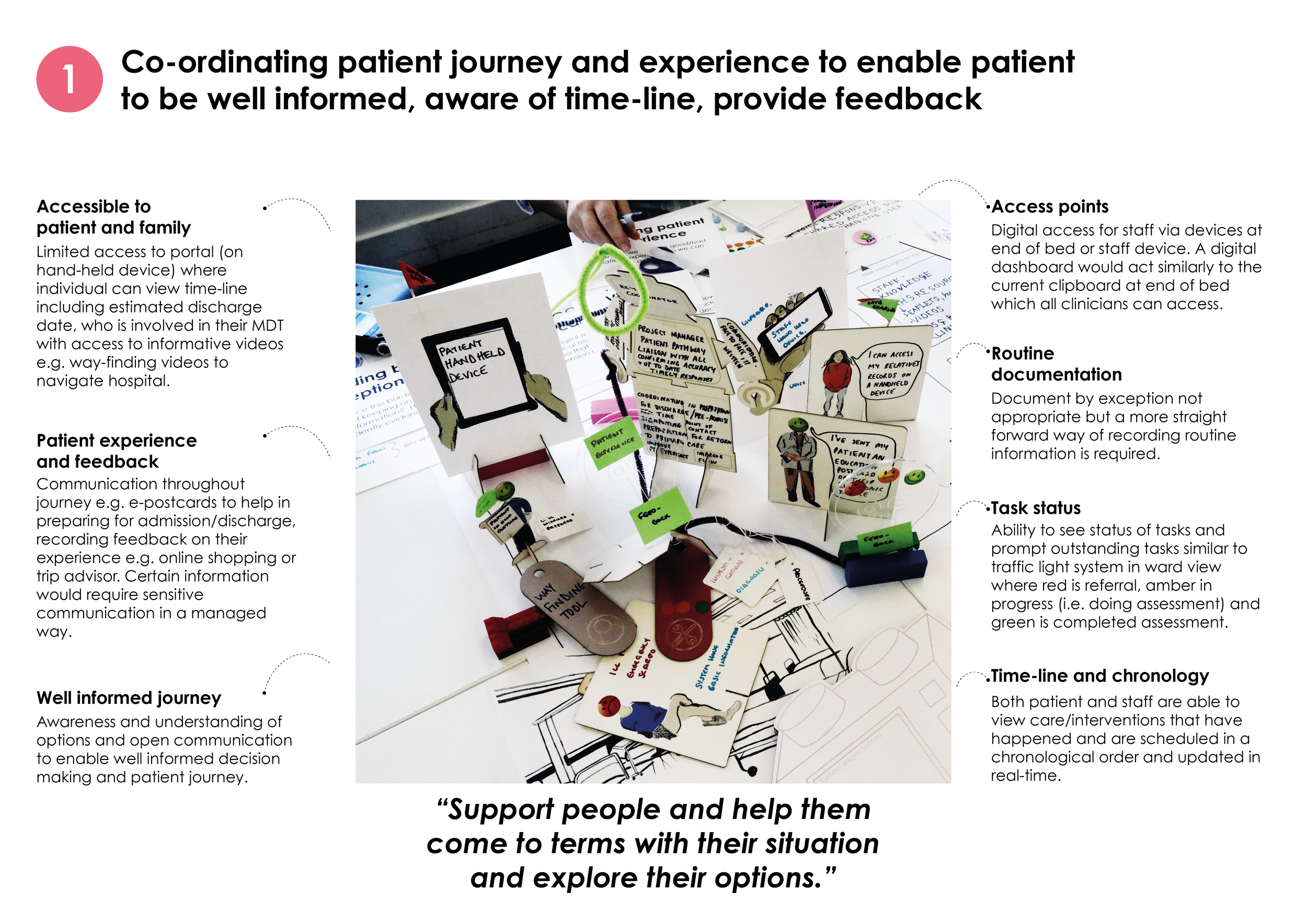
Using the idea of a story book, staff were asked to consider how they would aspire to work together to plan and deliver care centred around a person in the future without current constraints. Successive pages of the story were arranged along a patients journey: before being admitted as an in-patient; during admission; continuous care; discharge and; after an episode of care. A number of themes are detailed below and were developed into design briefs for subsequent design activities.
Preparation for patients
Participants discussed the need for patients to be aware of the expectation of them to prepare basics such as packing appropriately, labelling belongings and understanding that although they have been admitted for one condition there should be an expectation of treatment of others.
Giving the patient the option to review and/or raise details and submit specific information through some form of pre-admission suitable for the in-patient referral. This might include preliminary clinical information such as medical history, previous referrals, failure to attends, demographics, social circumstances and next-of-kin as well as alerts about the person e.g. psychiatric or allergies.
The ability of patients to self-manage as much as they are able to. Which would include anticipating needs and engaging with a range of services and support offered prior to admission that may be appropriate on discharge. During their episode of care participants described the need for a patient to engage with advice received through an ‘active recovery’.
Communicating decision-making
The methods for how to document decision-making and what information to capture were discussed. For example, documenting by exception or using voice recognition which also raised queries about how this would be audited. The system was the main point of discussion for coordinating care as it would allow communication with colleagues, the ability to share and build on colleagues’ documentation as well as alerting and provide search functions e.g. key words, shortcuts as well as links to standards of care, best practice statements and guidance.
Face-to-face conversation with colleagues will always be valuable in order to obtain detail however through the use of digital communication and sharing of data, staff could save more time for value-added discussions around planning of care.
Methods of communication with the patient such as a patient portal, verbal, patient diaries and an interactive patient board were suggested in order to share plans with patient and their families and allow the patient to communicate their experience. This might include a timetable of care and an estimated discharge date. However this does raise challenges around accessibility and security of information.
Coordinating the MDT team based on pre-assessment information
Participants discussed the preparation the staff could do before a patient admission in coordinating a team most appropriate to that persons needs and preferences. This might include providing the patient with information around speciality specific information e.g. who will be involved in their care and what to expect. Participants also wanted to know information prior to admission which informs a patient’s personal preferences around what and who is important to the person e.g. what matters to you and, getting to know you.
Key care coordinator role
Participants identified the importance of a coordinator role in managing one joint plan of care, monitoring this process and ensuring the person can understand what is communicated to them. Coordination of a core team could be assessed and adapted on a ‘needs-based’ approach which is informed by the pre-admission information and assessment of the patient. It was noted by one group of participants that quality indicators for those involved in the MDT would be required and could be self set per area.
A significant part of this role might be in the prioritising and vetting of knowledge and scheduling and ensuring this is visible and clear to all involved. Participants also discussed the involvement of a ‘key person’ in decision making which has been identified by the patient if they felt it would be beneficial to them.
Discharge planning at the point of admission
A key point of discussion across all groups was the need for early discussions about discharge and the involvement of other services to allow timely planning. A discharge summary or Core Discharge Document could be auto-populated along the patient journey, flagging activity and outstanding actions and contributing to timely discharges.
Training requirements
Professional respect and understanding of roles was also seen as a training need for a multi-professional team. Participants suggested training for staff on how to use the future record-keeping system in order to get the most benefit from the system, as well as training in communication with patients. Providing resources and sign-posting were also highlighted to support the staff’s aspirational ways of working.
Design briefs emerging from earlier design activity around the staffs preferred ways of working informed later design activities around the future record-keeping system. Participants were asked to choose a question(s) and develop these further into a future vision for the MDT record.
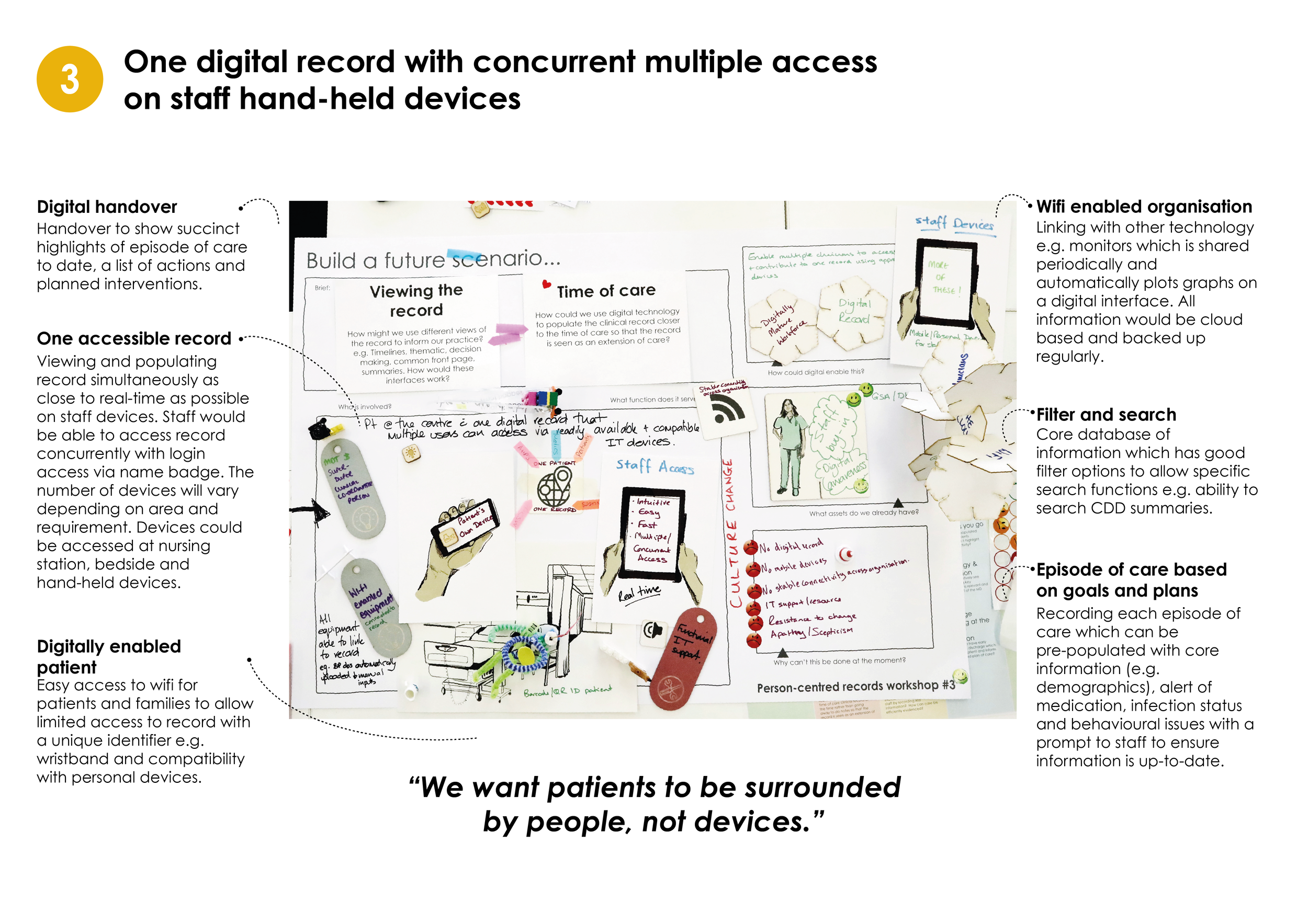
Digitally Enabled Ways of Working
Participants were asked to explore how digital records could support the interactions, relationships and communication of a multi-disciplinary team and their aspirational ways of working. With a re-framing of how they are working together, a re-framing of roles may also be required and so participants were asked to design the future workforce as a cast of characters, thinking about their role, the skills required and what contribution they would make to the MDT. Participants were then asked to construct future scenarios using the design briefs distilled from previous work and provided craft materials to build their vision. Participants then decided upon their expectations of the future system to support the scenarios.
Future workforce required to implement new processes for MDT working with the envisioned record keeping system
IN-PATIENT (AND/OR ACCOMPANYING PERSON)
An engaged, goal-oriented, prepared and realistic pro-active participant who is able to self-manage and take ownership of their care.Communication skills such as listening and questioning, in order to fully understand condition. Self-awareness, independence, planning skills and ability to use information IT skills (if contributing to the MDT electronic record directly) are important in order to self-manage.In-patients will be observant to their own condition with knowledge of who to turn to, knowledge of condition and provide accurate information in order to make informed choices.
CONTINUOUS INTERACTION
A MDT with constant and holistic in-patient presence to empower the in-patient to self manage and set goals and promote clinical, person-centred care with inter-professional roles and responsibilities such as assessing the patient; discovering needs; recording care; diagnosing and treating, and planning discharge.
SPECIALIST INTERACTION
An off-ward MDT to enhance clinical care at request of the on-ward MDT as required. Including providing: education for in-patient and in-patient staff; specialist skills and knowledge (e.g. surgery, medication); problem solving (e.g. knowledge of care services); links to off-ward services and specialist knowledge and skills.
CO-ORDINATOR
The co-ordinator will involve managing and facilitating the MDT through understanding the patient pathway and in-patient MDT common goals; referring and liaising with ‘as-required’ team and care services to co-ordinate and support an efficient and appropriate patient journey.
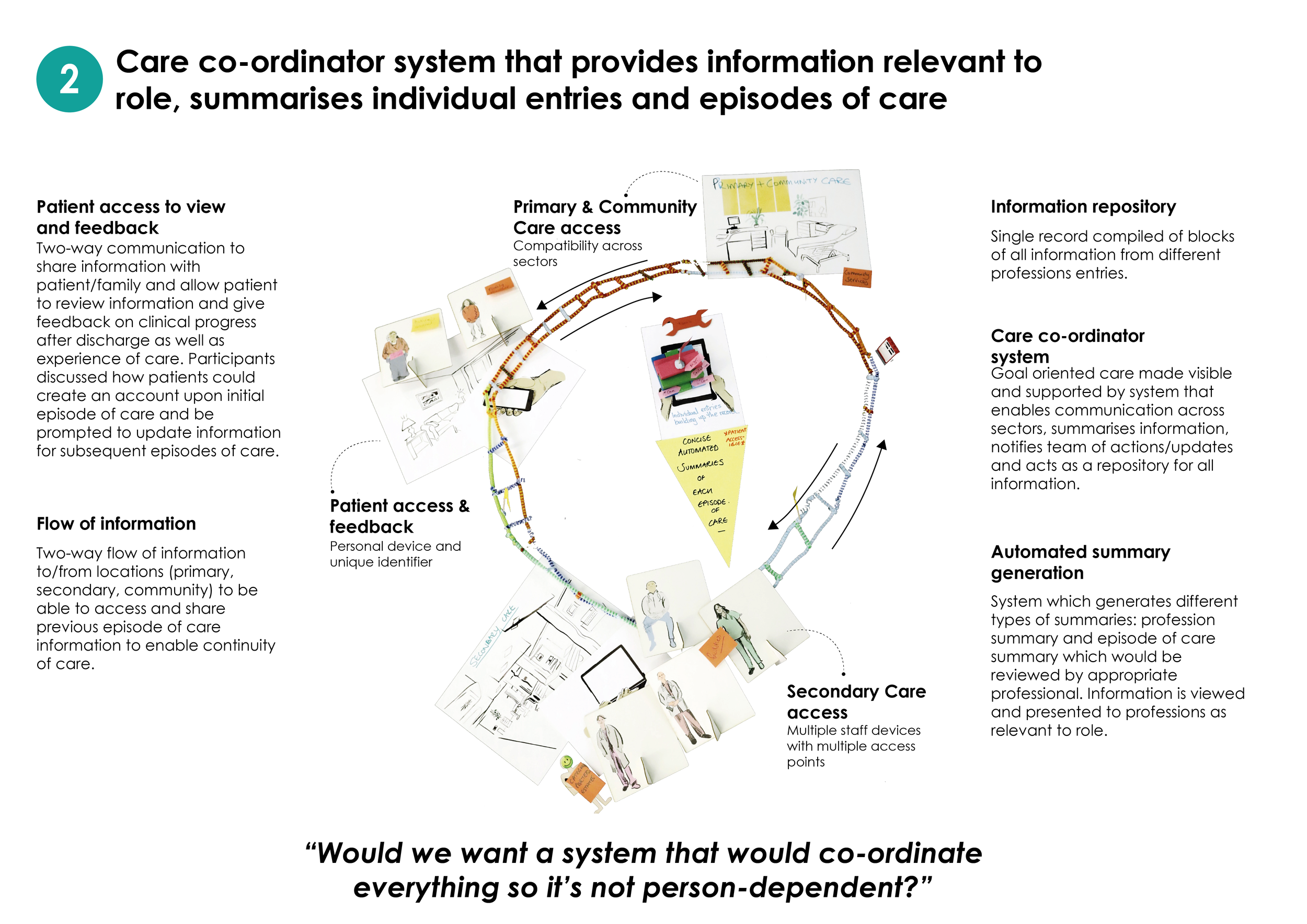
Future Scenarios
System Expectations
Following the co-design of the future scenarios above, participants were asked what they would expect a future electronic record system to do in order to support the participants’ preferred way of working. The expected features fall into three categories as below.
Non-clinical Expectations
Some expected features are non-clinical (i.e. could be found in most modern applications):
- filter and search functionality for previously captured information such as previous admissions, or profession specific information;
- a single interface that is user friendly and easy to use; access through any common device with concurrent multi-user access;
- 24/7 IT support;
- a visual timeline of activity and; automatic data collection where possible.
Unique Expectations
Views and features specifically to support the desired multidisciplinary way of working such as:
- profession specific areas but all can access;
- pre-populated views and forms with existing information where possible;
- unique identifier for access to appropriate level;
- and links to clinical guidance and best practice.
Features which support for inter-professional communication between in-patient staff such as a notifications and alerts system e.g. documents due, appointments, investigations,outstanding clinical tasks, etc.
There are also supporting features such as automatically generated summaries of a required type.
Out-of-scope Expectations
Although some subjects are currently out of this project’s scope, they are still of interest to the participants such as interfacing with primary care and local authority provided care systems and, equitable access for the patient. These subjects may inform future work.
Identified BARRIERS to MDT working
Trusting other staff’s assessments
Independent systems do not currently communicate
Unable to know what is going on in the community and the care services
Not everyone is patient goal focused
Lack of reliable connectivity (Wi-Fi)
Not enough electronic devices
No single patient record
“We’re all doing different things but we can’t see what anybody else is doing so we don’t have this match of roles and have no idea what’s going on.”
Identified Existing ASSETS for MDT Working
Skilled and knowledgable workforce
Assessments from other disciplines
Patient resources e.g. patient toolkit, NHS Grampian information resources
Transferable skills and sharing experience
“Our biggest asset is our workforce [...] So it’s about using folk to engage.
”
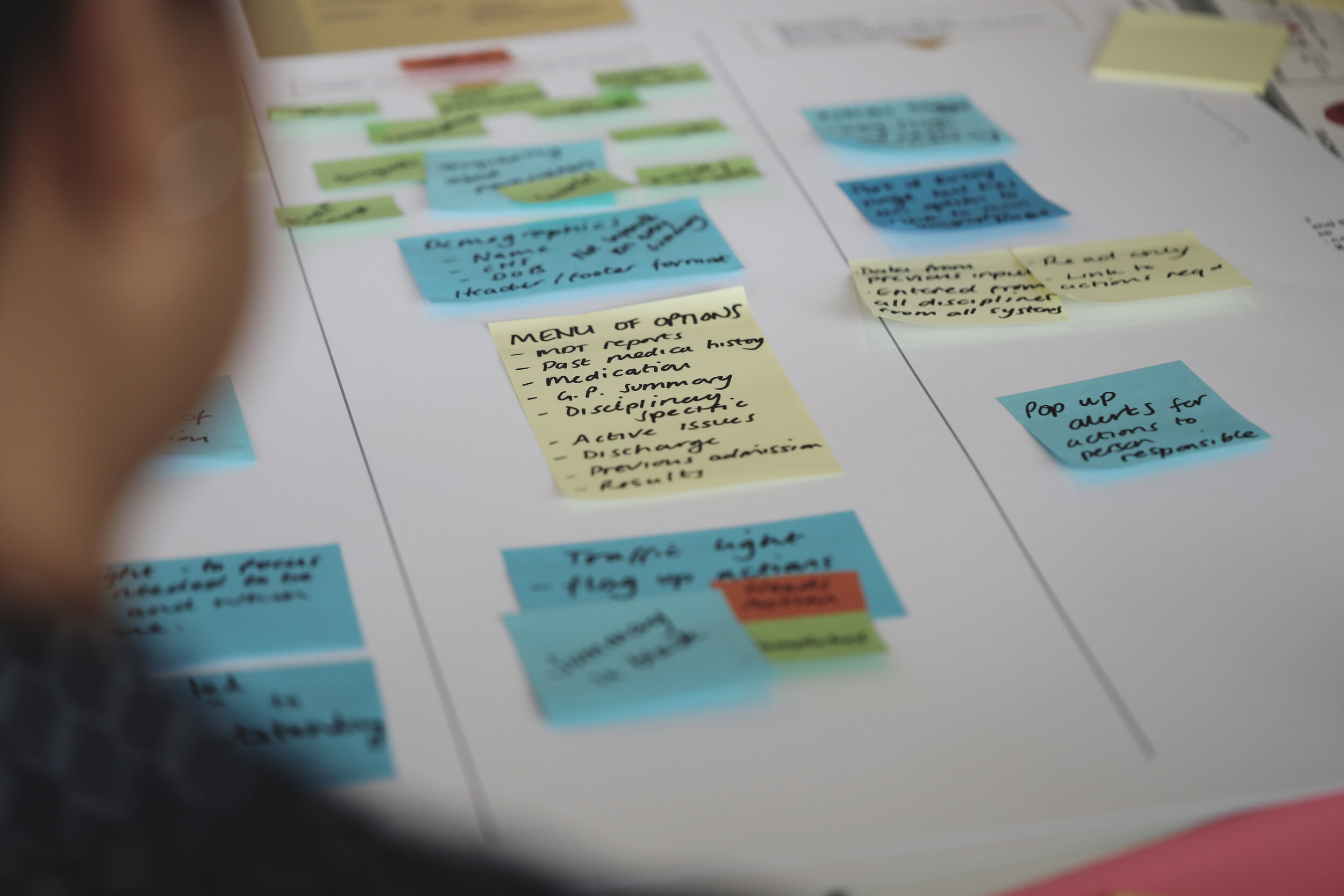
Defining the content of the future electronic record system
Towards the end of Q2, the focus moved towards defining requirements of a digital record-keeping system that would support the identified aspirational ways of working that is multi-disciplinary, considers the digitally enabled ways of planning care whilst also aligning with the design principles from Quarter 1. Participants were asked to make Priority Guides for the previously identified views of the record system as shown below. The participants chose to focus on the three highlighted views: a common ‘front page’; alerts and notifications for in-patient staff and; a mechanism for creating summaries. Priority Guides were used as a way to prototype views and features of the system without being distracted by the visual appearance of the final system. This is as opposed to designing wire-frames which can give the illusion of a considered and well defined prototype system by being visually appealing. The participants were first asked to consider the content of each view at a high-level (i.e. content headings) and rank each bit of content by importance to that particular view. Afterwards, participants were asked to co-design a detailed description of each view.
Showing ten potentially interesting views within the new electronic record-keeping system identified from the Planning Care co-design activities. The three highlighted views were chosen by the participants to be made into priority guides as below.
Priority Guides
Roadmap to reality
As we move from aspirational concepts towards requirements the participants were asked to think about how they might approach the realisation of the future system so as to ensure it is successful and overcomes some of the barriers highlighted in the Q1 report. A board game style tool was used to help guide the discussion through short, medium and long term goals and key moments along implementation. The main points were:
strategic planning
A strategic planning group needs to be established early on to ensure an appropriate approach to implementation with the involvement of all levels of staff including patients and governance to enable the realisation of a truly person-centred record that is potentially ‘once-for-Scotland’.
clear commitment and direction
Teams should be given the opportunity to figure out how they will change the way they work together. For this to happen a clear commitment is needed from NHS Grampian to back this system and when work should commence.
Introducing the workforce to the new system profession by profession, possibly starting with AHPs due to their working practice i.e. going away to write up their notes so this could be done electronically. If other professions then began to access the shared AHP notes within the new MDT record and saw its benefits they would potentially be less resistant to contributing to the single electronic record themselves.
Happy PATIENTS, HAPPY STAFF
In order for the future record keeping system to be successful, NHS Grampian need to ensure it works for everyone. Staff buy-in throughout the process is imperative to the success of introducing a person-centred record. Success should be measured in terms of how care is being improved.
‘half an hour to play’
When introducing the system, a ‘super duper’ user should receive the training first and then train colleagues. Staff should be given time to ‘play’ with the system and test it to gauge how much training would be required. This method of roll out in their own area would ensure staff buy-in and potentially reduce risks when introducing new ways of working.
Timeline of acivity in the 2nd Quarter of the Person-centred Records Project
NEXT STEPS
A further three design-led workshops are planned across the 3rd and 4th quarters with the aim of co-designing system requirements through prototyping in collaboration with software development professionals and simulating these in a training ward in order to validate, refine and demonstrate the preferable future system and working practice.
The research team at the GSA are planning to run a series of observation sessions on-ward with NHS Grampian in-patient staff to visually document staff interactions with the records e.g. using existing electronic and paper-based records during day-to-day activities. This will include the professionals’ interaction with in-patients. NHS research ethics approval for this activity is in process.
Finally (April 2020), recommendations for the preferred ways of MDT in-patient working and requirements for a new supporting electronic record-keeping system will be published here.
References
Ramsay, D., & Seth, P. (2017). Me to We. Introducing collaborative elements in the electronic record. BCMJ, 59(10), 507–5011.
Authored by Jay Bradley and Angela Bruce from the Digital Health & Care Institute/ Innovation School at the Glasgow School of Art, October 2019.